J Clin Sleep Med:打鼾睡眠不足可降低乳腺癌患者的生存期
2016-05-10 MedSci MedSci原创
J Clin Sleep Med:打鼾睡眠不足可降低乳腺癌患者的生存期来自华盛顿大学的一项新的研究表明,乳腺癌女性在确诊之前长期睡眠时间短并频繁打鼾则其预后较差,该研究成果已发表于Journal of Clinical Sleep Medicine。在美国,乳腺癌是女性最常见的癌症,其发病率仅次于皮肤癌。据美国癌症协会表示,今年美国有约246660名新发浸润性乳腺癌患者, 40000余名女性死于该
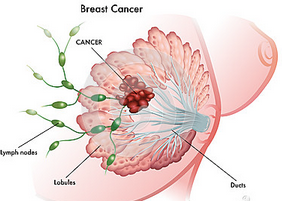
在美国,乳腺癌是女性最常见的癌症,其发病率仅次于皮肤癌。据美国癌症协会表示,今年美国有约246660名新发浸润性乳腺癌患者, 40000余名女性死于该病。
该研究领导者Amanda Phipps教授及其同事指出,既往研究已经表明睡眠质量差及睡眠时间短可增加癌症的发病风险。但是,研究并没有充分阐释睡眠与癌症结局之间的关系。
打鼾及睡眠时间短可增加两倍乳腺癌的死亡风险
该研究中,研究人员评估了某种睡眠特征是否会影响乳腺癌患者的生存期。
研究人员分析了21230名女性的数据,研究过程中所有女性均患有原发性癌症,但是癌症并没有扩散。
研究开始记录所有女性的睡眠时间,打鼾情况以及其他的睡眠特征。将这些数据与女性癌症结果的信息进行比较,以确定癌症的存活期是否受睡眠因素的影响。
结果发现,很少打鼾且每晚睡眠7-8小时的乳腺癌的女性相比,每周打鼾超过5晚睡眠时间不到6小时的乳腺癌女性死于癌症的风险至少高了两倍。校正影响因素后,睡眠特征仍可影响癌症生存期。
这些影响因素包括参与研究时参与者的年龄,癌症部位,婚姻状况,家庭收入,吸烟状况,身体活动状况,以及基线与癌症诊断之间的时间。
研究人员注意到,既往研究表明,睡眠问题可能会促进肿瘤的生长,减少癌症的生存期,这或许是因为睡眠不良影响了机体炎症反应的通路。
打鼾可能是影响癌症生存期的一个因素
该研究中,研究人员惊讶地发现打鼾可能与乳腺癌的生存期有关。
Phipps 说道:“据我们所知,以往并没有评估打鼾与癌症生存期之间的关联,但是我们的研究结果表明,打鼾则可能是影响癌症生存期的一个重要因素”。
研究人员认为他们的发现强调了充足的睡眠时间和良好的睡眠质量的重要性,特别是对于乳腺癌患者。
Phipps 还说道,“与影响癌症风险和癌症预后的其他因素不同,睡眠是一个机体可以控制的因素。我们的研究结果为优先保证睡眠质量提供了又一个理由。”
根据美国睡眠医学学会表示,成年人每天的睡眠时间应保证在7个小时左右,以避免与睡眠不足相关的健康风险的发生。
“健康、充足的睡眠对于机体幸福、公众健康和公共安全来说至关重要,”美国睡眠医学学会会长Nathaniel Watson博士说道,“所有的成年人都应将每天至少7小时的睡眠作为保持健康的首要事项。”
American Academy of Sleep Medicine news release, accessed 6 May 2016 via EurekAlert.
Additional source: American Academy of Sleep Medicine, Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society, accessed 6 May 2016.
Additional source: American Cancer Society, What are the key statistics about breast cancer?, accessed 6 May 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








文章真心很好,感谢作者
100
好文章,百姓也能从中学到好多医学知识
104
深入学习,好文值得点赞!
104
乏氧与肿瘤
115
#SLE#
73
#生存期#
51
#打鼾#
76
#乳腺癌患者#
57
#Med#
52