Nat Commun:遏制95%的前列腺癌细胞生长!新型药物问世!
2018-10-25 Michael,Zoe 转化医学网
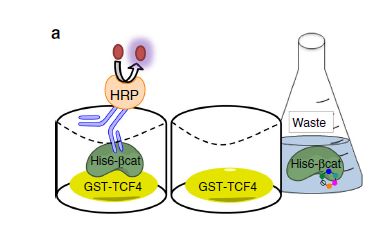
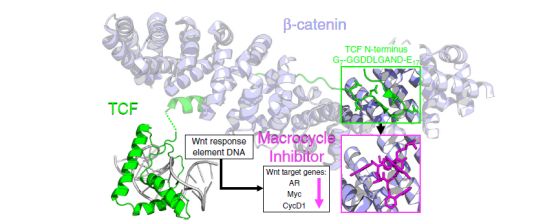
来自纽约大学的研究人员利用计算机辅助技术来研究新蛋白质—蛋白质间的相互作用,进而开发出一种全新的抗前列腺癌药物。该研究的最新研究发表于最新的《Nature Comunnications》杂志。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
49
#COMMUN#
48
学习
88
#癌细胞#
0
#新型药物#
65
#细胞生长#
60
#前列腺癌细胞#
46
学习了
84
是人们的一种希望
76
还没有开始实验还早呢!
74