J Am Geriatr Soc:英国研究称,≥80岁老人血压降至135 mmHg以下有害
2017-09-06 文韬 中国循环杂志
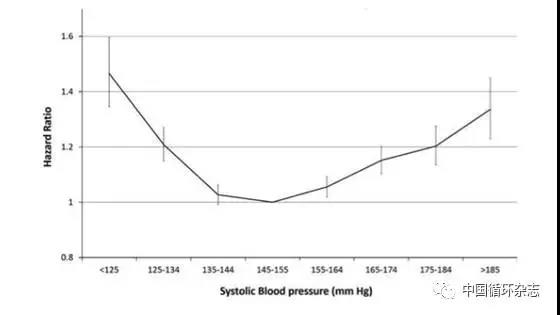
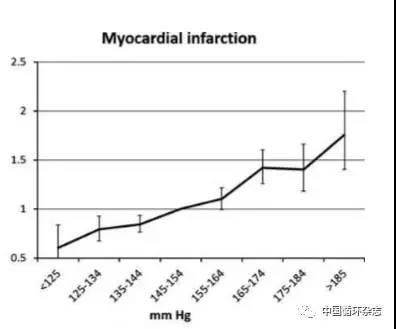
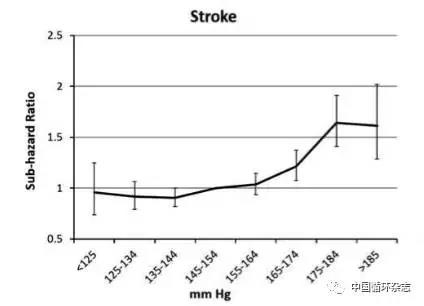
英国近期一项观察近8万人随访4年的研究发现,对于≥80岁的老年人,收缩压在于135~154 mmHg者的全因死亡率最低,而治疗后血压水平<135 mmHg者全因死亡率则增加25%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











对于老年人降压程度.又有了新证据.谢谢
81
#GER#
88
学习了受益匪浅
102
学习了
145
学习了受益匪浅
116
学习了
78
很好.学习了.很有帮助.
55
学习了谢谢了
59
英国近期一项观察近8万人随访4年的研究发现.对于≥80岁的老年人.收缩压在于135~154 mmHg者的全因死亡率最低.而治疗后血压水平<135 mmHg者全因死亡率则增加25%.
55
学习了很有用不错
73