JCEM:西那卡塞可减少透析患者重度甲旁亢发生
2013-10-21 desperado-c dxy
基线临床特征与重度持续性甲旁亢的关系 血液透析患者继发性甲状旁腺功能亢进(sHPT)的临床病程未被很好描述,而且,拟钙剂西那卡塞对sHPT疾病进展的影响尚不确定。为了描述接受磷酸盐结合剂和/或维生素D治疗患者的sHPT临床病程,以及西那卡塞对重度持续性HPT(定义为持续性甲状旁腺激素(PTH)浓度显著升高伴高钙血症或甲状旁腺切除)发生的影响,来自加拿大纽芬兰纪念大学Patrick
基线临床特征与重度持续性甲旁亢的关系
血液透析患者继发性甲状旁腺功能亢进(sHPT)的临床病程未被很好描述,而且,拟钙剂西那卡塞对sHPT疾病进展的影响尚不确定。为了描述接受磷酸盐结合剂和/或维生素D治疗患者的sHPT临床病程,以及西那卡塞对重度持续性HPT(定义为持续性甲状旁腺激素(PTH)浓度显著升高伴高钙血症或甲状旁腺切除)发生的影响,来自加拿大纽芬兰纪念大学Patrick S Parfrey教授及其团队进行了一项研究,该研究发现重度持续性HPT常在血液透析患者中发生,西那卡塞治疗可大幅减少其发生。该研究结果发表在2013年10月9日的The Journal of Clinical Endocrinology & Metabolism杂志上。【原文下载】
该研究是一项随机、双盲、安慰剂对照临床试验,在全球多个中心进行。从5755例血液透析患者中筛选3883例中到重度sHPT患者。主要评价指标包括:甲状旁腺切除术、重度持续性HPT、以及商品化西那卡塞的使用。干预措施包括:西那卡塞(每日30至180mg)或安慰剂治疗64个月。
该研究结果表明,1935例随机分配到安慰剂组的患者中,278例(14%)患者接受甲状旁腺切除术(手术前12月中PTH中位数为1872pg/ml)。年龄、性别、地域、合并症、钙(包含磷酸盐结合剂)的使用、以及基线血钙、血磷和PTH浓度与甲状旁腺切除术有关。443例(23%)例患者起始商品化西那卡塞治疗(治疗起始前PTH中位数为1108pg/ml)。
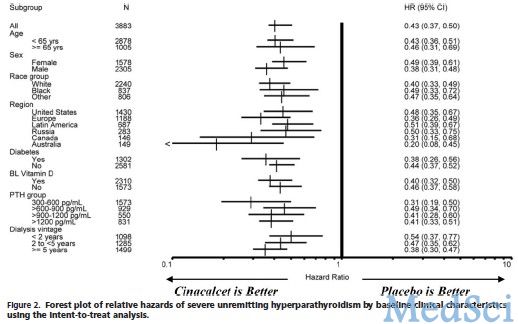
470例(24%)患者发生重度持续性HPT。在多元COX模型中,重度持续性HPT的相对危险度(随机分配到西那卡塞组的患者与随机分配到安慰剂组患者比较)为0.31(95%CI 0.26至0.37)。当校正基线临床特征后,这个相对危险度稍有差异。
该研究发现,重度持续性HPT常在血液透析患者中发生,而常规治疗和西那卡塞可大幅减少其发生。
原文检索:
Parfrey PS, Chertow GM, Block GA, Correa-Rotter R, Drüeke TB, Floege J, Herzog CA, London GM, Mahaffey KW, Moe SM, Wheeler DC, Dehmel B, Trotman ML, Modafferi DM, Goodman WG.The Clinical Course of Treated Hyperparathyroidism Among Patients Receiving Hemodialysis and the Effect of Cinacalcet: The EVOLVE Trial.J Clin Endocrinol Metab. 2013 Oct 9. 【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#西那卡塞#
77
#JCEM#
121
#JCE#
134
#透析患者#
74