BMJ:低密度脂蛋白与丹麦所有或特定死亡率之间的关联:前瞻性队列研究
2020-12-09 MedSci原创 MedSci原创
低密度脂蛋白胆固醇(LDL-C)是公认的引起动脉粥样硬化和心血管疾病发展的风险因素。许多降脂药疗效的随机对照试验都清楚地表明,降低LDL-C水平可有效降低将来发生动脉粥样硬
低密度脂蛋白胆固醇(LDL-C)是公认的引起动脉粥样硬化和心血管疾病发展的风险因素。许多降脂药疗效的随机对照试验都清楚地表明,降低LDL-C水平可有效降低将来发生动脉粥样硬化性心血管事件的风险。
LDL-C水平的降低能够减少心血管事件的发生,目前普遍的看法是,高水平的LDL-C与增加的死亡风险相关,而低水平的LDL-C却没有。 然而,一些有关LDL-C水平与所有原因致死风险之间关系的研究提供了相互矛盾的结果。有些研究显示出反直觉的逆相关性(随着LDL-C水平的提高,死亡率降低),而另一些研究则显示他们没有相关性。 这些研究大多数是在年龄较大的个体以及以历史人群为基础的队列中进行的。 另外,最近对未服用过降脂药的韩国年轻人群体的研究表明,LDL-C水平与死亡率之间呈U型关系。 因此,在一般人群中,LDL-C水平与所有或特定死亡率的风险之间的关联尚不清楚。 同样的,死亡风险最低的LDL-C的浓度也从未得到过相关证明。
Camilla Ditlev Lindhardt Johannesen等研究人员由此进行了一项前瞻性研究,他们随机选择了在丹麦国家民事登记系统内登记的108243名居民作为研究对象,使用Cox比例风险回归模型和连续量表(限制性三次样条),通过先验定义的百分位数类别对LDL-C的基线水平与死亡风险的关联性进行评估。主要结果是所有原因导致的死亡率。 次要结局是引起特定死亡率(心血管,癌症和其他死亡率)的原因。
他们发现,在108243位20至100岁的人中,有11376位(10.5%)在研究期间死亡,中位年龄为81岁。LDL-C水平与所有原因致死风险的相关性呈U型。与LDL-C浓度为3.4-3.9 mmol / L(132-154 mg / dL; 61-80百分位数)的个体相比,LDL-C浓度低于1.8 mmol / L(<70 mg / dL; 1至5个百分位数)的个体和的LDL-C浓度高于4.8 mmol / L(> 189 mg / dL;96至100百分位数)的个体,他们的所有病因死亡率多变量调整风险比在所有人群中分别为1.15(95%置信区间1.05至1.27)和1.25(95%置信区间1.15至1.36) 。与LDL-C浓度为2.3 mmol / L(89 mg / dL)并接受降脂治疗的个体相比,在普通人群和未接受降脂治疗的个体中,死亡风险最低的LDL-C浓度为3.6 mmol / L(140 mg / dL)。这一结果在各年龄段的男性和女性中未观察到明显差异。而任何程度的LDL-C水平的升高都与心肌梗死的风险增加有关。
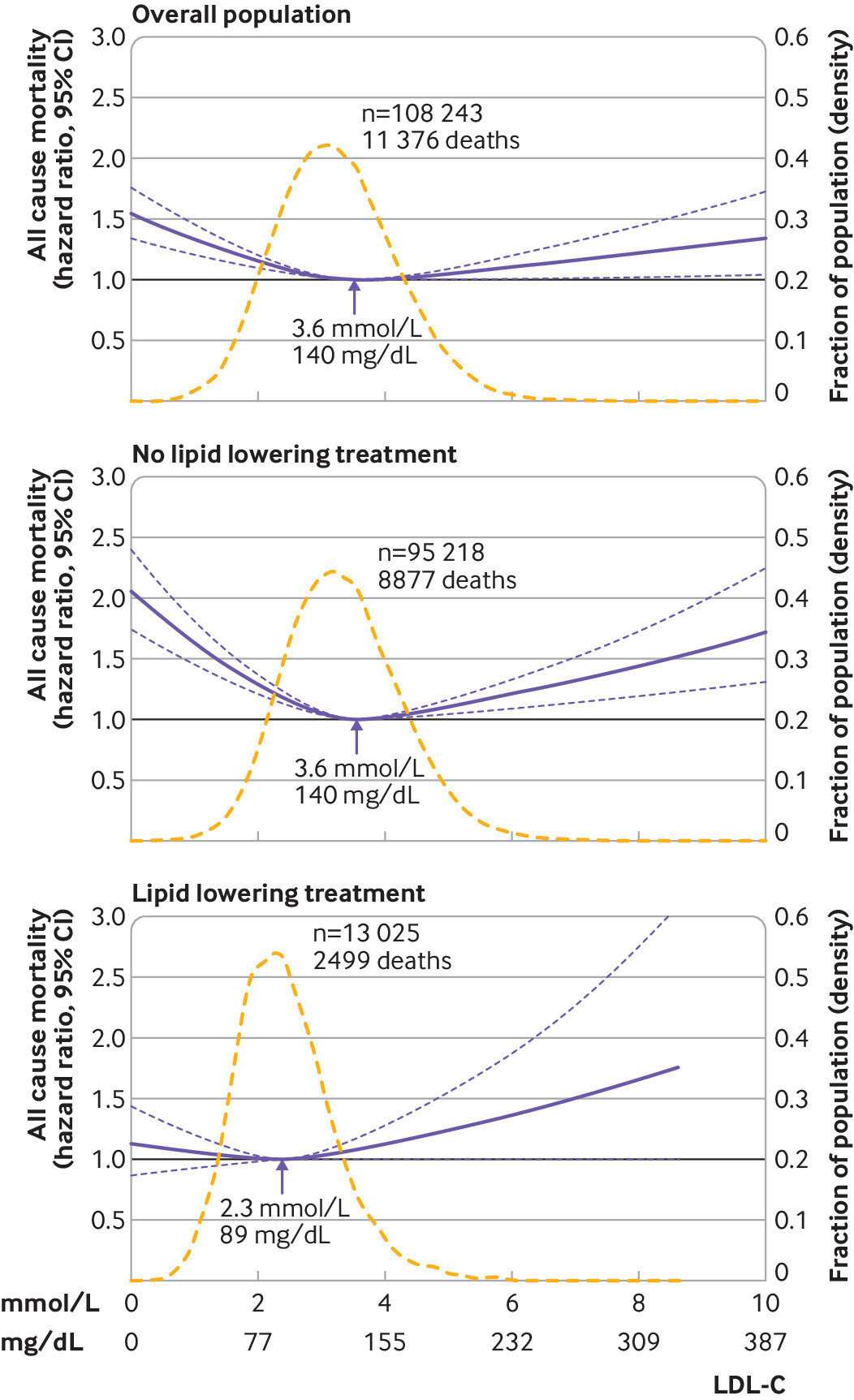
除外心血管疾病,低或高水平的LDL-C都会导致死亡风险的增加,例如癌症等。在普通人群中,LDL-C浓度为3.6 mmol / L(140 mg / dL)的人群寿命最长。 如果本实验的结果能够在更多研究中得到证实,这一发现将对临床和公共卫生产生重要影响。
原文链接:https://www.bmj.com/content/371/bmj.m4266
BMJ 2020; 371 doi: https://doi.org/10.1136/bmj.m4266 (Published 08 December 2020)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
49
#前瞻性队列研究#
67
#前瞻性队列#
50
#前瞻性#
47
学习了学习了!!
104
学习
114
学习
100
学习了
0
学习了
106
学习
72