Eur Heart J:早期心脏转甲状腺素淀粉样变的特征和自然病程
2022-05-26 MedSci原创 MedSci原创
I期的ATTR-CM患者可根据诊断时NT-proBNP浓度和利尿剂需求进一步进行分层。尽管短期和中期生存率良好,但Ia期ATTR-CM患者心血管疾病发病率显著升高。
转甲状腺素淀粉样心肌病(ATTR-CM)患病率日益升高,尽管根据尸检系列的患病率估计,心脏有ATTR淀粉样沉积的患者中,只有一小部分患者被诊断为心脏淀粉样变性。由于ATTR-CM的诊断具有挑战性且经常被遗漏,因此真正的疾病患病率仍然未知。

ATTR-CM越来越多地在疾病早期被诊断出来,被国家淀粉样变性中心(NAC)定为为I期ATTR-CM。但是目前对早期ATTR-CM的自然史仍缺乏足够的了解和归纳。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员对879例ATTR-CM患者进行了回顾性多中心观察性研究,这些患者要么为野生型TTR基因型,要么携带p.V142I TTR变异体,在通过NAC ATTR I期生物标记物诊断时未接受淀粉样变疾病的治疗。通过Cox回归分析,研究人员发现诊断时与死亡率独立相关的疾病特征包含了B型利钠肽前体N末端(NT-proBNP)、TTR基因型和肌钙蛋白T。患者被分为NAC ATTR Ia期,定义为呋喃塞米等效利尿剂需求量<0.75 mg/kg和NT-proBNP≤500 ng/L或伴有心房颤动时≤1000 ng/L,NAC ATTR Ib期包括所有其他的I期患者。
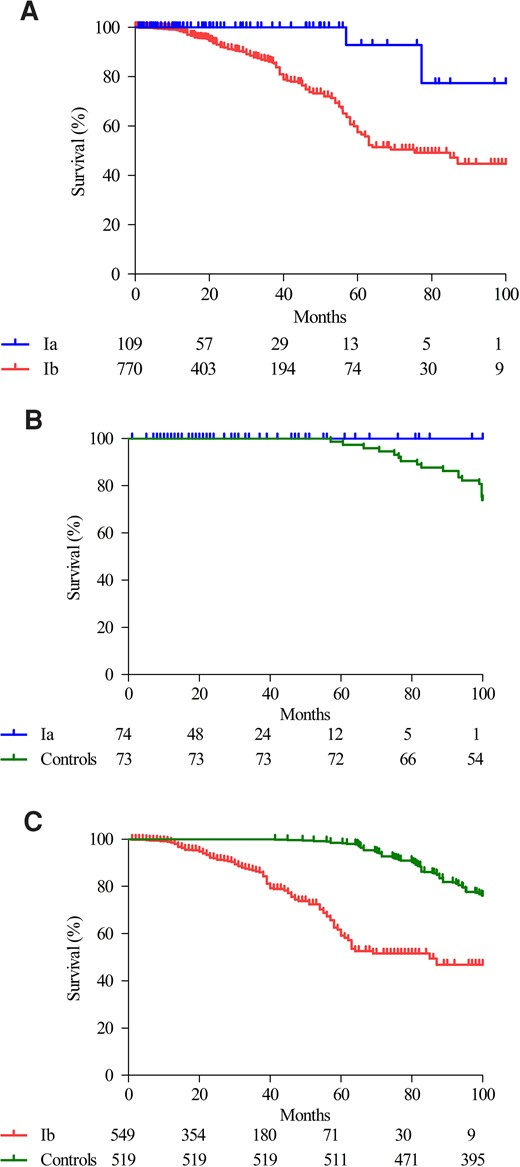
88%的NAC ATTR Ib期患者估计的中位生存期为75(95%可信区间为57-93)个月,而12%的Ia期患者估计的中位生存期100个月以上[死亡风险比为5.06(95%可信区间为1.23-20.87);P=0.025],尽管在诊断时心血管疾病发病率显著增加,但在随访期间,包括在确诊为NAC ATTR Ia期的患者中,心血管疾病发病率有所增加。英国NAC ATTR Ia期患者的估计生存率与英国普通人群对照组相当(P=0.297)。
由此可见,NAC ATTR I期的ATTR-CM患者可根据诊断时NT-proBNP浓度和利尿剂需求进一步进行分层。尽管短期和中期生存率良好,但Ia期ATTR-CM患者心血管疾病发病率显著升高。
原始出处:
Steven Law,et al.Characteristics and natural history of early-stage cardiac transthyretin amyloidosis.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac259/6591080.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#自然病程#
54
#ART#
45
#淀粉样变#
53
#HEART#
35