Oncotarget:重磅!科学家鉴别出肝癌的天然抑制蛋白
2017-05-10 生物谷 生物谷
日前,一项刊登在国际杂志Oncotarget上的研究报告中,来自奥古斯塔大学的研究人员通过研究发现,一种能够帮助细胞进行有序组织并且完成任务的关键蛋白或许是预防肝癌的一种肿瘤抑制子。这种名为Scrib的蛋白质会根据癌症类型作为肿瘤抑制蛋白和癌基因而出现,在肝癌中该蛋白往往会从细胞的保护外层迁移进入细胞内部发挥作用,一旦进入细胞内部,该
日前,一项刊登在国际杂志Oncotarget上的研究报告中,来自奥古斯塔大学的研究人员通过研究发现,一种能够帮助细胞进行有序组织并且完成任务的关键蛋白或许是预防肝癌的一种肿瘤抑制子。这种名为Scrib的蛋白质会根据癌症类型作为肿瘤抑制蛋白和癌基因而出现,在肝癌中该蛋白往往会从细胞的保护外层迁移进入细胞内部发挥作用,一旦进入细胞内部,该蛋白的表达就会增加,同时还会抑制三种促进肝癌发生的癌基因进行表达。
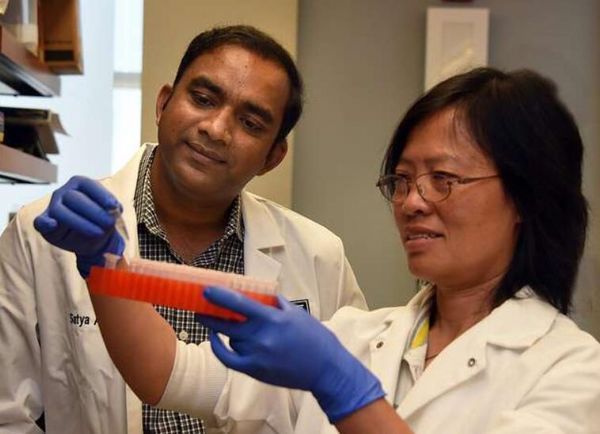
图片摘自:Phil Jones
分子生物学家Satya Ande表示,这项研究中我们首次发现,在肝癌中,当细胞开始癌变时,Scrib蛋白能够转移到细胞质和细胞核中;Scrib能够作为肿瘤抑制蛋白尽力抑制癌细胞的生长。同时本文研究首次给出证据表明,在人类和动物的肝癌中Scrib能够充当肿瘤抑制蛋白的角色。
Scrib蛋白通常会驻留在细胞膜中来维持细胞极性;研究者Ande说道,在肝癌中我们发现有些Scrib蛋白会依然停留在细胞膜中,但有些Scrib蛋白却会移动到细胞质以及细胞核中,一旦该蛋白发生移动其就能够发挥作用来抑制Yap1, c-Myc和cyclin D1三种癌基因的表达。当仅对对Scrib蛋白进行重定位并且增加其表达并不会消除小鼠模型中的肿瘤时,研究者发现小鼠机体的肿瘤变小了,低水平的Scrib大白会增强动物模型中肝脏肿瘤的生长,但高水平的Scrib则能够抑制培养液中肝癌细胞的生长;而且研究者也并未在Scrib缺失的小鼠机体中发现自然发生的肝癌出现,这也就表明该蛋白在肝脏中并不扮演正常的角色。
更有意思的是,研究者还发现,在其它某些类型的癌症中,Scrib蛋白的运动以及其表达量的增加是其促进癌症发生的标志。下一步研究人员将通过更为深入的研究来阐明Scrib作为肝癌抑制蛋白的重要性,目前研究人员发现在30例所研究的人类肝脏肿瘤中,有70%的肿瘤中Scrib蛋白的表达都会增加,而在不同癌症中,该蛋白似乎扮演着不同的角色,比如,低水平的Scrib似乎能够减缓淋巴瘤发生的开端,但同时研究者在结肠癌、前列腺癌以及乳腺癌中也发现了低水平的Scrib蛋白,在这些癌症中,Scrib能够移动到细胞质中促进癌症发展,当然这至少是在动物模型中的研究结果。
最后研究者表示,Scrib蛋白似乎在大部分癌症中表达水平较高,后期我们还将通过更为深入的研究来阐明其在多种癌症中扮演的角色以及如何利用该蛋白开发治疗多种人类癌症的新型疗法。
原始出处:
Scrib protein identified as a natural suppressor of liver cancer
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#target#
70
新发现,希望对临床有用,谢谢分享
86
#重磅#
60
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。点赞啦!
102
继续学习。
108