Nat Med:单独atezolizumab或者atezolizumab结合贝伐单抗与舒尼替尼在肾细胞癌中治疗的临床活性和相关分子响应比较研究
2018-06-10 AlexYang MedSci原创
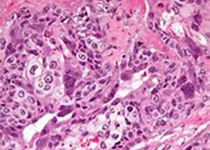
最近,有研究人员阐述了 IMmotion150的研究结果,该研究是一个随机的阶段2研究,具体包括了305名从未治疗过的转移性肾细胞癌患者,并且利用单独的atezolizumab(anti-PD-L1)或者结合贝伐单抗(anti-VEGF)与舒尼替尼治疗结果的比较。主要结果为在意向治疗中的无进展自由生存(PFS)和PD-L1+群体。研究发现,atezolizumab+贝伐单抗或者atezolizum
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#mAb#
85
#Nat#
91
#细胞癌#
93
学习一下谢谢
95
#贝伐#
79
#Med#
53