JACC:2014版高血压防控专家意见对当前心血管临床治疗的意义:NCDR PINNACLE 注册处的观点
2014-12-01 MedSci译 MedSci原创
背景:自2003年以来,JNC-7(全国联合委员会第七次报告)一直是血压管理的主要指南。2014年专家组建议提高60岁及以上患者,以及患有糖尿病或慢性肾病病人的血压控制目标值。目的:本研究的目的是检验2014年专家组的血压管理的建议对于美国门诊部心血管病人治疗的影响。方法:采用全国心血管数据注册PINNACLE的数据,我们评估了符合2003和2014专家意见定义的高血压病人的比例,并找到血压目标值
背景:自2003年以来,JNC-7(全国联合委员会第七次报告)一直是血压管理的主要指南。2014年专家组建议提高60岁及以上患者,以及患有糖尿病或慢性肾病病人的血压控制目标值。
目的:本研究的目的是检验2014年专家组的血压管理的建议对于美国门诊部心血管病人治疗的影响。
方法:采用全国心血管数据注册PINNACLE的数据,我们评估了符合2003和2014专家意见定义的高血压病人的比例,并找到血压目标值变化了的患者。
结果:在1185253例患者中,706859(59.6%)按照2003版 JNC-7的标准血压控制已达标。以2014版专家建议为标准,880378(74.3%)患者的血压控制达标。在173519例(14.6%)血压目标值变化的人里,40323(23.2%)之前发生过一次中风或短暂性脑缺血发作,112174(64.6%)有冠状动脉疾病。此外,这组的Framingham平均危险评分为8.5±3.2%,10年动脉粥样硬化性心血管疾病的风险评分为28±19.5%。
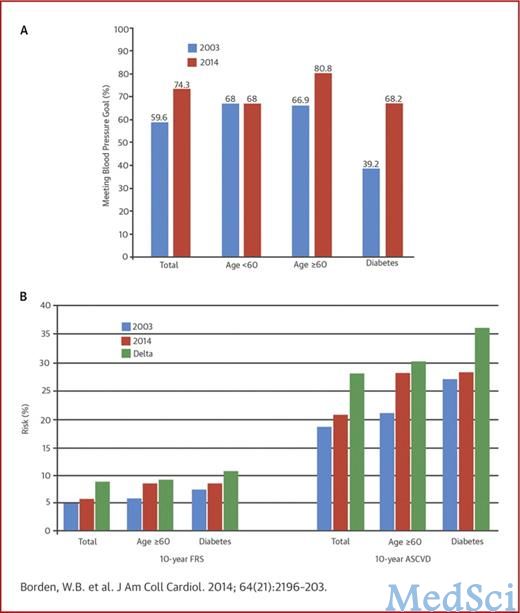
结论:美国门诊部患有高血压的心血管患者,将近七分之一在JNC-7建议中没有实现治疗目标,却已满足2014版本指南的治疗目标。如果新的建议在临床实践中运用,血压的达标与心血管事件都需要仔细监测,因为许多患者的目标血压现在更宽松,却存在较高的心血管病风险。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JACC#
39
#ACC#
59
#临床治疗#
62
#注册#
42