血管内介入取栓治疗静脉窦血栓1例
2020-05-07 李克磊 洪景芳 望家兴 中国微侵袭神经外科杂志
蚌埠医学院附属联勤保障部队900医院2018年3月采用上矢状窦取栓术治疗1例上矢状窦血栓继发脑出血病人,报告如下。
蚌埠医学院附属联勤保障部队900医院2018年3月采用上矢状窦取栓术治疗1例上矢状窦血栓继发脑出血病人,报告如下。
1.病历摘要
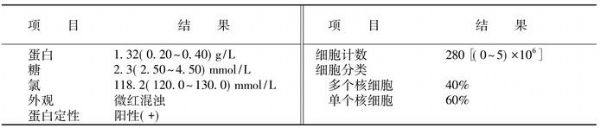
女,70岁;无明显诱因出现头痛及左侧肢体乏力,外院CT提示左侧颞顶叶少量血肿,考虑为高血压性脑出血,并给予保守治疗。2d后意识障碍加重,无法对答,右侧肢体肌力下降。复查CT提示左侧颞顶叶血肿较前明显增大,CTA提示:上矢状窦后2/3段及双侧横窦显影差,考虑静脉窦血栓形成。
遂转入本院,入科查体:神志不清,GCS评分9分,双侧瞳孔等大等圆,直径约3.0mm,对光反射灵敏,颈部抵抗(-),左侧肢体肌力Ⅳ级,右侧肌力Ⅱ级,肌张力正常,双侧病理征阴性。
入院CT提示左侧颞顶叶血肿(图1A),临时给予低分子肝素钠注射液0.4ml,皮下注射,并行DSA显示:上矢状窦后2/3段及双侧横窦不显影,上矢状窦前1/3段显影良好,经额顶叶皮质静脉、外侧裂静脉向海绵窦引流(图1B)。
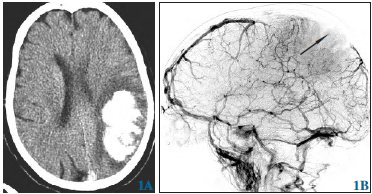
图1 血管内介入取栓治疗上矢状窦血栓继发脑出血。1A术前CT示:左侧颞顶叶血肿增多;1B右侧颈内静脉造影显示:上矢状窦后2/3段及双侧横窦均不显影(箭头);
遂行上矢状窦介入取栓术(图1C~1E):取左侧腹股沟韧带下约1.5 cm股静脉穿刺点,经静脉鞘送入6F导引导管至左侧颈内静脉内,Rebar18微导管在微导丝的导引下进入上矢状窦内,经反复手推造影剂,明确血栓的位置,然后通过导管释放Solitaire6mm×30mm支架,5min后回收支架,取出部分陈旧性血栓。反复2次操作后,再次造影,提示上矢状窦显影较前改善,但窦内仍有少许充盈缺损(图1F),遂将微导管留置于上矢状窦血栓处,持续泵入尿激酶进行接触性溶栓。
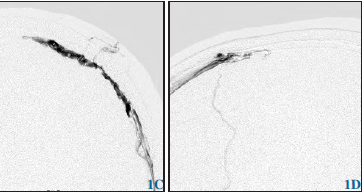
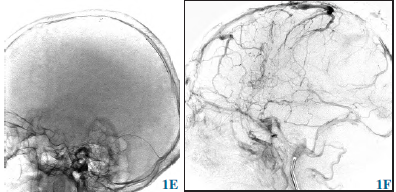
图1C、1D在上矢状窦内不同位置反复手推造影剂,明确血栓位置;1E将Solitaire支架经乙状窦进入上矢状窦内,取血栓;1F取栓后右侧颈内静脉造影示:上矢状窦及横窦显影较前明显改善;
术后第2天复查头部CT,提示颅内血肿无明显变化(图1G)。术后3d内的主要治疗药物:①0.9%氯化钠50ml+尿激酶30U,2次/2d,微导管泵入。②低分子肝素钠注射液0.4ml,2次/d,皮下注射。术后第4天复查DSA,提示上矢状窦及双侧横窦显影较前明显好转(图1H)。然后给药改为:①低分子肝素钠注射液0.4ml/次,2次/d,皮下注射。②口服华法林钠片3.75mg/次,1次/d;随访血INR值。
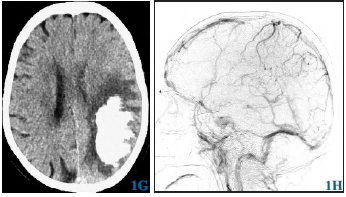
图1G术后第2天复查CT示:脑内血肿较前无变化;1H术后第4天右侧颈内动脉造影示:上矢状窦及横窦均显影
出院时查体:神志清楚,对答切题,右侧下肢肌力Ⅳ级,右侧上肢肌力Ⅲ级,左侧肢体肌力正常。出院后长期口服华法林,定期复查血INR值。随访1个月,术后病人恢复良好,双侧肢体肌力Ⅴ级,无明显后遗症。
2.讨论
尽管血管内介入治疗技术在不断发展,但仍有约15%的CVST病人死亡或生活不能自理。其中3%~15%死于急性期,主要死亡原因是脑疝。对于CVST,现阶段公认的首选治疗方式为抗凝治疗,即阻止血栓进展,促进血栓溶解及血管再通,预防深静脉血栓或肺栓塞,同时认为即使病人就诊时已合并颅内出血,仍可不作为抗凝治疗的禁忌证。
对伴随颅高压症状的脑出血病人,若不及时开通静脉回流降低颅内压力、减轻脑水肿,则有再出血风险,此时仅行抗凝治疗无法达到理想疗效,可采用血管内介入治疗和(或)减压术辅以全身抗凝的方式治疗。静脉窦血栓继发脑出血行血管内介入机械取栓术报道甚少。刘佳雨等报道10例表现为蛛网膜下腔出血的颅内静脉窦血栓,经过抗凝治疗1年后,完全再通6例,部分通畅、皮质侧支循环明显改善4例。
蒋云等报道22例静脉窦血栓,其中2例为脑实质出血,给予抗凝治疗,效果不明显后再联合溶栓治疗。本例与前述报道的不同点在于,病人意识障碍严重,脑实质出血量大(约36ml),急需解决静脉高压导致的持续性脑出血,而且要防止因治疗导致新发出血。实施机械取栓术可以快速打通阻塞的静脉窦,恢复静脉引流,而且大大降低抗凝及溶栓药物的使用量,减少球囊扩张、溶栓等导致脑出血的风险。
术中可以多次取栓,但要防止栓子脱落等严重并发症。术后病人恢复良好。介入取栓术适用于已经发生颅内出血或其他治疗方法无效的急性或亚急性脑静脉系统血栓形成病人,在有介入治疗条件的医院,介入取栓术可以作为一种治疗方法。
LI等回顾性分析52例静脉窦血栓病人的资料,其中39例伴有脑出血,提出机械取栓术和溶栓治疗严重静脉窦血栓病人是安全有效的。DASHTI等提出静脉窦内机械取栓术可以作为静脉窦血栓的一线治疗。ZUURBIER等报道10例静脉窦血栓合并脑出血病人,经单纯去骨瓣减压术及抗凝治疗,术后4例出现脑内出血量增加。
综上所述,介入机械取栓术治疗严重静脉窦血栓继发脑出血病人可获得良好效果。
原始出处:
李克磊,洪景芳,望家兴,王守森.血管内介入取栓治疗静脉窦血栓1例[J].中国微侵袭神经外科杂志,2019(04):180-181.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好
89
#血管内介入#
55
#静脉窦血栓#
57
#静脉#
62
#取栓#
76
#静脉窦#
57