Nature:科学家发现前列腺癌扩散的遗传指纹
2017-01-10 李易潇 bio360
1月10日凌晨,来自加拿大的科学家发表在《Nature》上的研究报告他们发现了前列腺癌的遗传指纹,这可以作为局部手术疗法或放疗治疗后前列腺癌复发的指标,这一研究结果可以帮助临床医生的个性化诊断和靶向性治疗。加拿大研究人员已经发现了前列腺癌的遗传指纹,解释了为什么高达30%可治愈的局部前列腺癌患者在放疗或手术后,会发展成为扩散的侵袭性疾病。遗传指纹分析,也称基因标定或基因鉴定,是一种使用通过比较DN
1月10日凌晨,来自加拿大的科学家发表在《Nature》上的研究报告他们发现了前列腺癌的遗传指纹,这可以作为局部手术疗法或放疗治疗后前列腺癌复发的指标,这一研究结果可以帮助临床医生的个性化诊断和靶向性治疗。
加拿大研究人员已经发现了前列腺癌的遗传指纹,解释了为什么高达30%可治愈的局部前列腺癌患者在放疗或手术后,会发展成为扩散的侵袭性疾病。
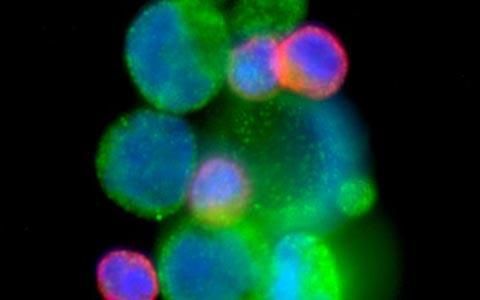
遗传指纹分析,也称基因标定或基因鉴定,是一种使用通过比较DNA片段来区别不同个体的方法。前列腺癌是临床上常见的一种上皮性恶性肿瘤。在全世界范围内,前列腺癌发病率在男性所有恶性肿瘤中位居第二。虽然大多数前列腺癌患者是局部、可治愈的,但是每年全世界仍有超过20万男性由于前列腺癌转移而死亡。在美国前列腺癌的发病率已经超过肺癌,成为第一位危害男性健康的肿瘤。前列腺癌很容易扩散,遗传是前列腺癌发展成临床型的重要危险因素。
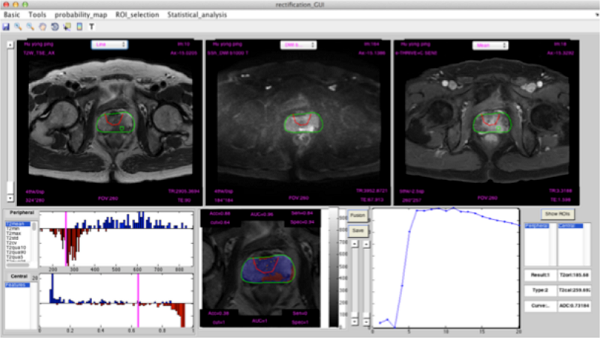
玛嘉烈公主癌症中心的Robert Bristow和安大略癌症研究所的Paul Boutros团队是该文章的共同研究者。研究人员分析了500名加拿大非遗传性前列腺癌患者的局部肿瘤,为了更好地了解患者的疾病发展进程,研究人员使用先进的DNA测序技术检测前列腺癌的遗传学变化。另一项相关的研究也发表在今天的《自然通讯》上, Bristow和Boutros破解了遗传密码,揭示为什么男性在遗传了影响细胞中DNA损伤修复的BRCA2基因突变后,BRCA-2遗传病在特定的情况下会发展成致命性疾病。
遗传指纹分析具有很高的准确性,能够精确分辨手术或放射治疗后发展良好的患者,以及那些在早期已经发生前列腺外扩散的患者。解释了为什么在放疗或手术后,有高达30%的可能治愈型局部前列腺癌的患者发生扩散侵袭性疾病。“这些信息为我们提供了关于前列腺癌患者治疗反应的新的精确度,并为如何更好地治疗前列腺患者、提高整体治愈率提供了重要线索,”Bristow博士说。
此外,除了今天发表的两个研究,Bristow团队在前列腺癌的研究中取得了很多成果。早在2014年发表在《Lancet Oncology》的研究就开发出了一种新型的遗传检测手段,其可以帮助检测患高风险前列腺癌患者在手术或放疗后疾病复发的风险。2015年《Nature Genetics》上的研究中阐明了前列腺癌患者机体癌症病灶中的多种患处的分子特性。
研究人员表示下一步是将这项研究结果转化为可用于临床的分子诊断工具。Bristow博士说:“我们将在接下来的两三年内完成对500多名男性的研究,这是一个令人兴奋的前列腺癌研究时代,在临床上我们很快就能够鉴定出患者的癌症确切遗传状态,根据病人的反应相应治疗,以治愈世界范围内更多的前列腺癌患者。”
原始出处:
1. Genomic hallmarks of localized, non-indolent prostate cancer. Nature, 2017.
2. Germline BRCA2 mutations drive prostate cancers with distinct evolutionary trajectories. Nature Communications, 2017.
3. First molecular portrait of localized, multi-focal prostate cancer and a new gene subgroup driving it . Nature Genetics, 2015.
4. Development of a genetic test to identify which men are at highest risk for their prostate cancer to recur after localized treatment with surgery or radiotherapy . Lancet Oncology, 2014.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#指纹#
70
#科学家发现#
54
#Nat#
48
前列腺癌患者机体癌症病灶中的多种患处的分子特性。
70
帮助临床医生的个性化诊断和靶向性治疗。
69
继续学习
63
文章很好,经常阅读
74