JAMA Neurol:血清N-乙酰氨基葡萄糖或是多发性硬化疾病进展的重要标志物
2021-06-01 MedSci原创 MedSci原创
血清N-乙酰氨基葡萄糖缺乏或是进展型多发性硬化的重要生物标志物,GlcNAc缺乏可能与MS患者的进展性疾病和神经退行性变有关

多发性硬化症(MS)是炎症脱髓鞘引起的神经功能障碍,而进展型MS(PMS)的特点是持续炎症、再髓化失败和进展性神经退行性变,最终导致不可逆的神经残疾。一般而言,复发缓解型MS患者 (RRMS)转化为继发进展性MS(SPMS)需要近20年,但其中,大约10%的患者从一开始即为原发性进展型MS (PPMS)。N-聚糖是构成细胞表面受体的重要组成,其在小鼠模型中,N-聚糖缺乏会促进炎性脱髓鞘、减少髓鞘化和神经退行性变。N-乙酰氨基葡萄糖(GlcNAc)是N-聚糖形成的限速底物,近日研究人员考察了多发性硬化患者内源性聚糖血清水平与MS症状的相关性。

本次研究为在美国和德国的2个研究中心进行的横断面验证研究,在2010年4月20日至2013年6月21日期间从门诊招募MS患者和健康对照者,分析血清样本中GlcNAc及其立体异构体N-乙酰己糖胺(HexNAc)的水平,并将其与影像学和临床疾病标志物相关联。
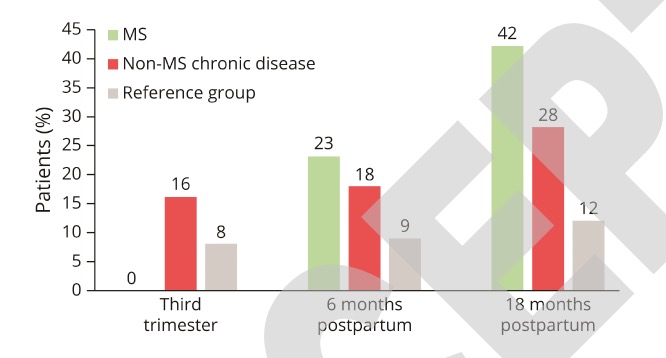
开发队列包括66名健康对照者(38名女性;平均年龄42岁),33例复发缓解型MS(RRMS)患者(25名女性,平均年龄50岁),21例进行型多发性硬化(PMS)患者(14名女性,平均年龄55岁)。验证队列包括125名RRMS患者(83名女性;平均年龄40岁),55例PMS患者(女性22例;平均年龄49岁)。在开发队列中,对照组GlcNAc及其立体异构体(HexNAc)的平均血清水平为710nM,RRMS患者为682nM,而PMS患者与健康对照组和RRMS组相比,GlcNAc水平显著降低(548nM)。在验证队列中, RRMS组与PMS组之间,GlcNAc及其立体异构体差异显著(709 vs 405nM)。与影像学和临床疾病标志物相关联后,较低的HexNAc血清水平与更差的扩展残疾状态量表评分、下丘脑容积减小和视网膜神经纤维层变薄相关,而低基线HexNAc水平与18个月时脑容量损失严重程度百分比相关。
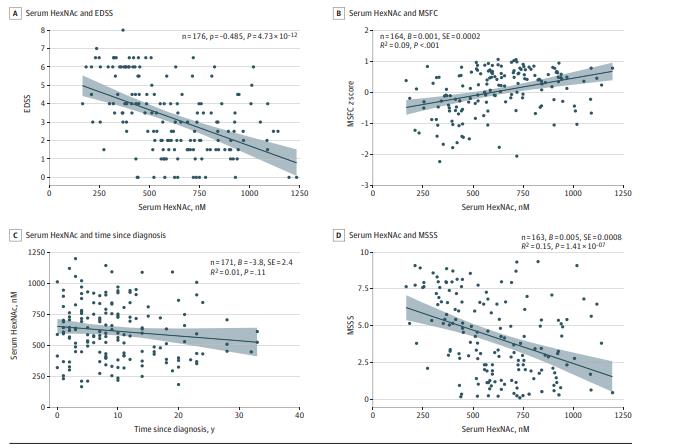
HexNAc水平与MS临床症状
研究认为,血清N-乙酰氨基葡萄糖缺乏或是进展型多发性硬化的重要生物标志物,GlcNAc缺乏可能与MS患者的进展性疾病和神经退行性变有关。
原始出处:
Alexander U. Brandt et al. Association of a Marker of N-Acetylglucosamine With Progressive Multiple Sclerosis and Neurodegeneration.JAMA Neurol. May 10,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多发性#
88
#标志物#
86
#疾病进展#
73
#Neurol#
77
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
90
学习了,谢谢分享
99