J Hypertens:糖尿病对女性的危害更大
2017-09-17 聚焦高血压编辑部 聚焦高血压
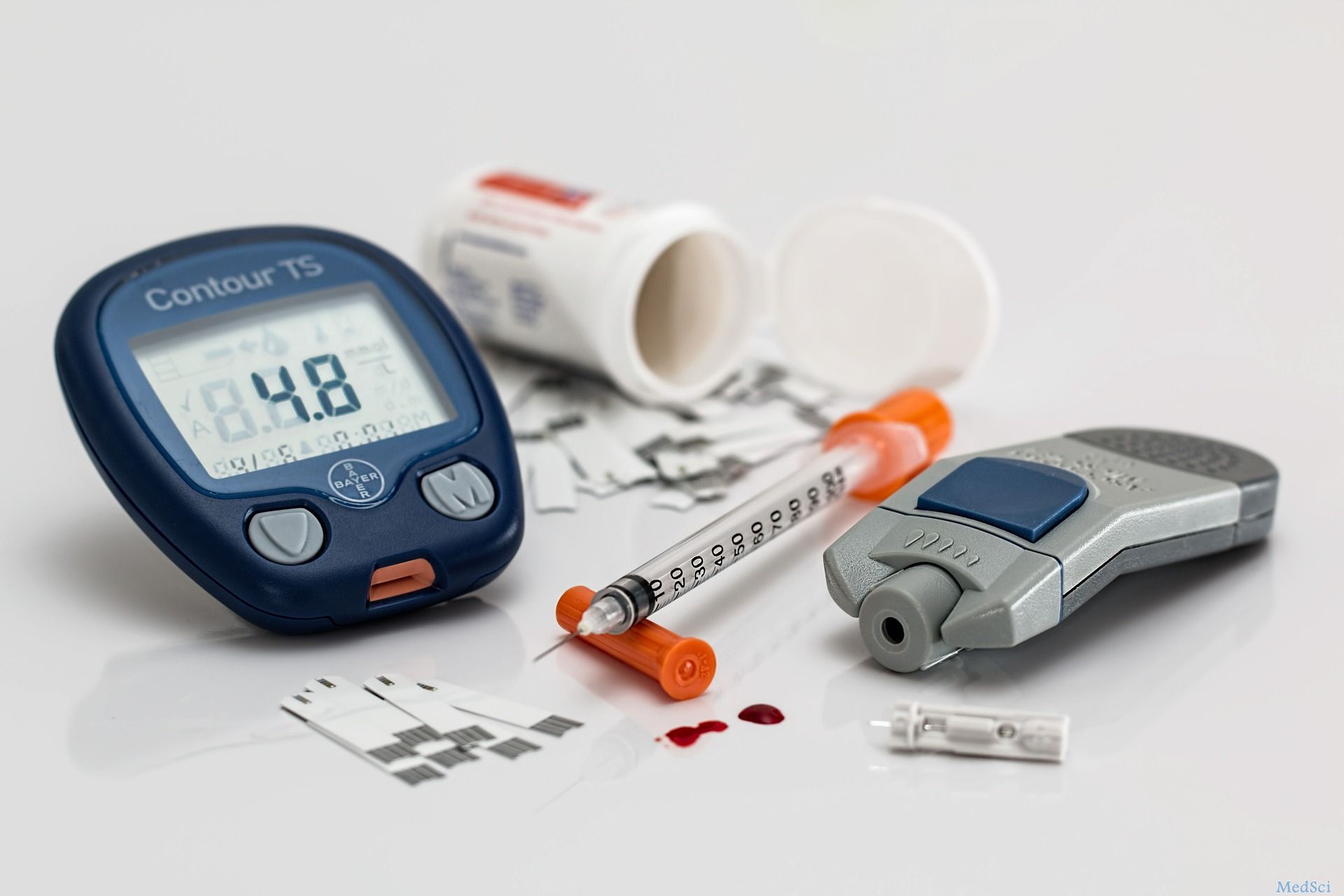
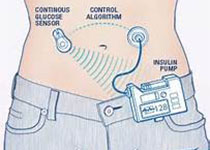
既往有研究证明,男性更容易患糖尿病,但糖尿病对女性的危害更大。糖尿病与性别之间确实存在交互作用吗?来自法国、比利时、瑞典、智利等国的研究者,收集了7个随机对照试验的数据,共计3万多例患者个体的数据,通过分析多个心血管终点事件,试图回答上述问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
57
#TENS#
58
糖尿病应该更早发现.控制.
100
学习了谢谢分享
95
学习了.涨知识
113
学习了.谢谢
103