Nat Med:转移性乳腺癌中Durvalumab与维持化疗的疗效比较
2021-01-21 xiaozeng MedSci原创
乳腺癌包括三种主要的分子亚型,即Her2过表达、激素受体阳性(HR+)和三阴性乳腺癌(TNBC)。 HR+和Her2过表达的转移性乳腺癌(mBCs)目前可通过靶向疗法(内分泌疗法,CDK4/6抑制剂和
乳腺癌包括三种主要的分子亚型,即Her2过表达、激素受体阳性(HR+)和三阴性乳腺癌(TNBC)。 HR+和Her2过表达的转移性乳腺癌(mBCs)目前可通过靶向疗法(内分泌疗法,CDK4/6抑制剂和Her2抑制剂)进行转化治疗。
抗PD-L1抗体能够抑制PD1介导的免疫抑制信号转导。既往的多项II期临床试验显示,部分mBC患者可从这些免疫疗法中获益。最近的一项化疗与抗PD-L1抗体联合使用的III期试验显示,对转移性TNBC患者的无进展生存期(PFS)具有中等疗效。然而,目前尚不清楚在转移性乳腺癌患者中抗PD-L1单药抗体作为维持疗法的功效。
该研究报告了一项II期随机试验SAFIR02-BREAST IMMUNO的结果和生物标志物分析,该试验比较了抗PD-L1抗体(durvalumab,度伐利尤单抗)与Her2阴性mBC患者的维持化疗之间的效果。
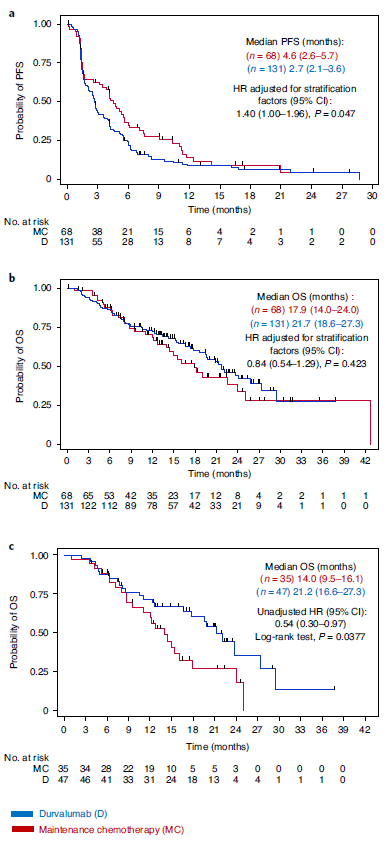
Kaplan-Meier分析患者的无进程生存期和整体生存率
该研究主要招募了Her2阴性的转移性乳腺癌患者病例,患者在经过6至8个化疗周期后疾病仍未出现进展。共199名患者被随机分为durvalumab组和维持化疗组。研究显示,durvalumab并不能改善患者的无进展生存期以及整体生存率(OS)。
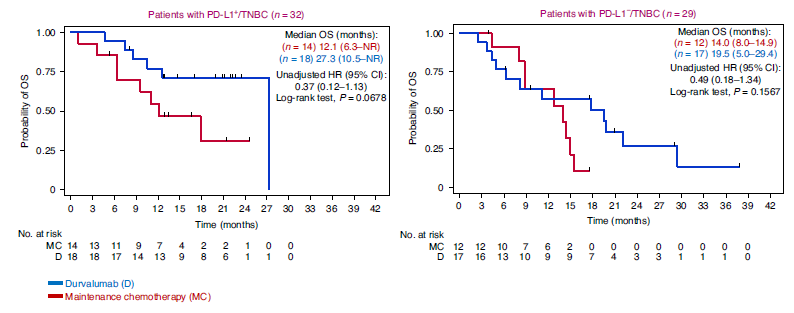
在一项探索性亚组分析中,durvalumab能够改善三阴性乳腺癌患者的OS。探索性分析显示,PD-L1+TNBC患者(n = 32)的死亡风险比(HR)为0.37,而PD-L1- TNBC患者(n = 29)为0.49。TNBC患者的探索性分析显示,具有CD274基因增益/扩增的患者(n = 23)的durvalumab功效(OS)HR为0.18。而CD274基因正常/丢失的患者(n = 32)的HR为1.12。
Kaplan-Meier分析PD-L1的表达对TNBC患者总生存率的影响
淋巴细胞(CD8、FoxP3和CD103表达)浸润和同源重组缺陷的肿瘤并不能通过探索性分析预测对durvalumab的敏感性。由于只有一名患者出现种系BRCA突变,因此该发现应谨慎解释。
总而言之,该研究结果为评估TNBC患者维持治疗中durvalumab的单药治疗提供了依据。探索性分析确定了CD274基因的扩增为潜在的敏感性生物标志物。在激素受体阳性和Her2阴性的患者中,维持化疗比durvalumab更有效。
原始出处:
Bachelot, T., Filleron, T., Bieche, I. et al. Durvalumab compared to maintenance chemotherapy in metastatic breast cancer: the randomized phase II SAFIR02-BREAST IMMUNO trial. Nat Med (18 January 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
123
#Nat#
87
期待更好的结果
124
#转移性#
103
#Med#
130
#TNBC#患者#维持治疗#中#Durvalumab#的单药,在激素受体阳性和Her2阴性的患者中,维持化疗比durvalumab更有效。这需要进一步研究!
261
谢谢梅斯提供这么好的信息,学到很多
100
挺有意思
123