Cancer Research:基因组守护者的叛变:最强抑癌基因p53,竟会促进肝癌发展
2022-07-16 王聪 “生物世界”公众号
该研究发现了一种新的机制——抑癌基因 p53 的表达竟会自相矛盾地促进慢性肝病患者的肝癌发展。慢性肝病(CLD)患者肝细胞中 p53 的持续激活实际上可以促进肝癌的发展。
自1979年被发现以来,p53 基因一直是肿瘤学研究的焦点之一。在 Pubmed 数据库中用 p53 为关键词搜索,可以找到超过十万篇文献。在 Nature 杂志2017年的一项统计中,p53 基因以绝对优势位列过去几十年最热门研究基因榜第一名。
在多种肿瘤中,p53 是一个拥有广泛而强大功能的抑癌基因,被誉为“基因组守护者”。p53 会响应细胞中的各种应激源(例如DNA损伤)而被激活。p53 的激活会促进 DNA 修复,或促进异常的细胞受控死亡,从而阻止癌症的发生和发展。因此,p53 基因突变在许多癌症中非常常见,超过一半的癌症患者携带了 p53 基因突变。p53 基因的突变是癌症发生、发展、治疗耐药性和预后不良的重要驱动力。
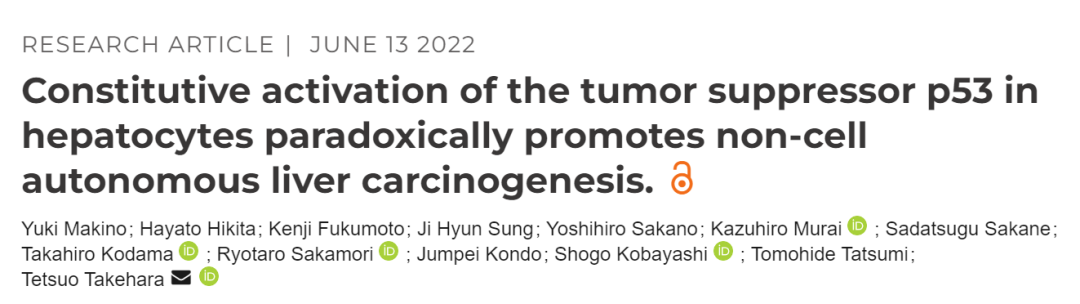
近日,日本大阪大学的研究人员在 Cancer Research 期刊发表了题为:Constitutive activation of the tumor suppressor p53 in hepatocytes paradoxically promotes non-cell autonomous liver carcinogenesis 的研究论文。
该研究发现了一种新的机制——抑癌基因 p53 的表达竟会自相矛盾地促进慢性肝病患者的肝癌发展。慢性肝病(CLD)患者肝细胞中 p53 的持续激活实际上可以促进肝癌的发展。
慢性肝病(CLD)可由多种不同因素引起,包括病毒感染、饮酒和脂肪堆积等,所有这些因素都可以诱导 p53 激活。之前的研究表明,p53 在慢性肝病患者的肝细胞中处于恒定的激活状态。然而,尚不清楚这在慢性肝病的病理生理学中起什么作用。
研究团队表示,临床数据清楚地表明,p53 在慢性肝病患者的干细胞中被激活,而 p53 是人体预防肿瘤形成的重要组成部分,因此,p53 在慢性肝病中的作用就变得更加耐人寻味了。
为了进一步探索这个问题,研究团队构建了在肝细胞中积累 p53 的肝癌小鼠模型(携带 KRAS-G12D突变),这是通过敲除 MDM2 基因来实现的,MDM2 蛋白能够靶向降解 p53 蛋白。研究团队发现,这些肝细胞积累 p53 的小鼠出现了肝脏炎症、肝细胞凋亡和衰老相关分泌表型(SASP)增多,SASP 可导致附近细胞癌变。而该研究显示,具有 p53 积累的小鼠确实增加了肝癌的发展。
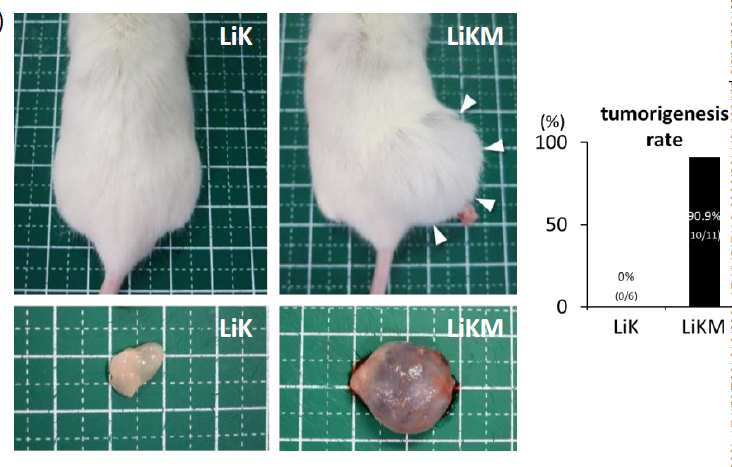
研究团队还观察到这些 p53 累计的小鼠具有干细胞样特征的肝祖细胞(HPC)数量增加。研究团队分离这些 HPC 细胞,培养后注射到实验小鼠皮下时,这些小鼠会长出肿瘤,这表明 HPC 在 p53 累计的小鼠的肿瘤形成中发挥关键作用。
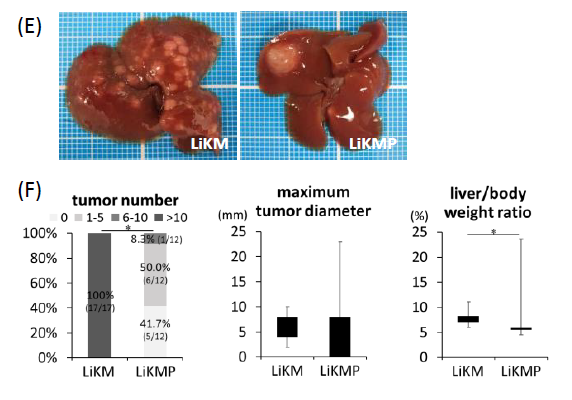
然而,当研究人员进一步敲除小鼠模型中的 p53 基因后,肝癌加速发展和其他相关表型不再发生。这说明 p53 激活在肝癌发生发展中发挥了重要作用。
最后,研究团队将182名慢性肝病(CLD)患者和23名健康者的肝脏样本进行了比较,结果显示,慢性肝病(CLD)患者的肝脏活检样本显示,激活的 p53 表达与细胞凋亡水平、衰老相关分泌表型(SASP)、肝祖细胞(HPC)相关基因表达,以及后来的癌症发展呈正相关。
根据这些试验结果,研究团队总结道:在慢性肝病(CLD)患者的干细胞中激活的 p53 可以创造一个支持肝祖细胞(HPC)形成肿瘤的微环境。这提出了一个新的肝癌发生机制,作为最著名的抑癌基因,p53竟会促进肝癌的发生。这些结果也提示了 p53 是慢性肝病患者潜在的癌症预防治疗靶点。
原始出处:
Yuki Makino, Hayato Hikita, Kenji Fukumoto, et al. Constitutive activation of the tumor suppressor p53 in hepatocytes paradoxically promotes non-cell autonomous liver carcinogenesis. Cancer Res canres.4390.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑癌#
58
#抑癌基因#
65
#p53#
75
#癌基因#
69
#Research#
51