ACG 2016:诊断性静脉切开术可影响肝硬化患者的血红蛋白水平
2016-10-30 MedSci MedSci原创
据ACG 2016上展示的一项新的研究显示,研究住院肝硬化患者出血与其血红蛋白和红细胞压积水平的变化有关。肝硬化患者本身出血的风险很高,因此,即使是最轻微的血红蛋白的增加都可引起出血。研究人员共纳入了482名肝硬化成人患者,最终分析了312名患者(平均年龄为56±10岁;64%为男性;89%为白种人)。评估的变量包括住院期间总失血量,血管的数目和类型,住院至出院期间血红蛋白的变化。平均住院天数为8
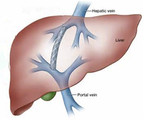
据ACG 2016上展示的一项新的研究显示,研究住院肝硬化患者诊断性静脉切开术与其血红蛋白和红细胞压积水平的变化有关。
肝硬化患者本身出血的风险很高,因此,即使是最轻微的血红蛋白的增加都可引起出血。
研究人员共纳入了482名肝硬化成人患者,最终分析了312名患者(平均年龄为56±10岁;64%为男性;89%为白种人)。
评估的变量包括住院期间总失血量,住院至出院期间血红蛋白的变化。平均住院天数为8天。
入院时患者的平均血红蛋白为10.5 ± 2.3 g/dL,出院时为 9.4 ± 1.7 g/dL,相应的平均差值为–1.1 ± 1.7 g/dL。平均失血量为183±174毫升,平均输血1.7±0.4个单位。
入院时的年龄和血红蛋白的水平,以及出血量可通过单因素分析预测血红蛋白的变化,但是并不能预测住院时间。多变量分析中校正多个变量后,出血量仍是预测血红蛋白下降的一个强有力的因素(P<0.0001)。
了解血红蛋白的预期变化,以及诊断性放血有助于指导观察这些患者的贫血及进一步的研究。
原始出处:
Melinda Stevens. Diagnostic phlebotomy impacts hemoglobin in cirrhosis. Healio, October 27, 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
56
#诊断性#
50
#ACG#
59
???
55
新内容,值得学习
66
好棒的分享
48
学习了,说不定以后可以研究学习
61
学校了。白种人和黄种人区别很大的。数据只能供参考。
66
学习新知识谢谢。
39
血红蛋白的预期变化,诊断性放血有助于指导观察这些患者的贫血。
34