JAMA Surg:腹腔内温热化疗可提高腹膜假黏液瘤患者术后生存率
2021-02-02 MedSci原创 MedSci原创
对于腹膜假黏液瘤患者,在肿瘤细胞减灭术后进行腹腔内温热化疗可显著提高患者生存率
腹膜假黏液瘤(PMP)是发生在腹腔壁层、大网膜及肠壁浆膜面的低度恶性黏液性肿瘤,发病率较低,主要表现为腹围进行性增加伴腹胀,手术治疗为主,很少转移,但难以治愈、易复发,复发者预后不佳。腹腔内温热化疗(HIPEC)在控制胃癌术后腹腔内游离癌细胞播散方面有一定效果。近日研究人员考察了HIPEC对腹膜假性粘液瘤患者预后的影响。
研究分析了PSOGI队列数据,包括1924例阑尾黏液囊肿性PMP患者,患者在肿瘤细胞减灭术(CRS)基础上,随机接受HIPEC治疗或对照, HIPEC组治疗方案包括奥沙利铂-氟尿嘧啶-亚叶酸、顺铂-丝裂霉素、丝裂霉素-奥沙利铂。研究的主要终点包括总生存率、严重并发症、二次手术以及30天和90天死亡率。
1924名患者参与研究,其中男性占51.8%,平均年龄56岁,376名患者仅接受CRS治疗,1548名患者接受CRS-HIPEC联合治疗。仅接受CRS治疗患者的年龄较大(平均年龄:60 vs 54岁),淋巴结受累较少(14例[3.7%] vs 119例[7.7%]),先前接受过术前全身化疗的比例较高(198例[52.7%]vs 529例[34.2%]),肿瘤组织学分类高度的比例较高(179 例[47.6%]vs492 例[31.8%])。除丝裂霉素治疗方案外,HIPEC不会增加手术风险,但术后并发症风险更高(HR=1.99)。在所有亚群中,HIPEC治疗后的总体存活率显著提高(校正危险比[HRs],0.60-0.68)。CRS-HIPEC组5年加权总生存率分别为57.8%,而CRS单独治疗组为46.2%(加权HR:0.65),其中HIPEC方案采用奥沙利铂-氟尿嘧啶-亚叶酸(HR:0.42)和顺铂-丝裂霉素方案(HR:0.57)的效果最为显著。
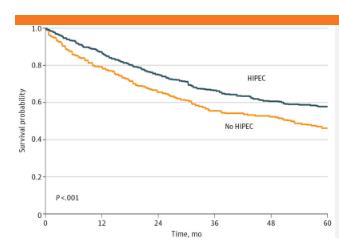
研究认为,对于腹膜假黏液瘤患者,在肿瘤细胞减灭术后进行腹腔内温热化疗可显著提高患者生存率。
原始出处:
Shigeki Kusamura et al.The Role of Hyperthermic Intraperitoneal Chemotherapy in Pseudomyxoma Peritonei After Cytoreductive Surgery.JAMA Surg. January 27, 2021.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#腹腔内#
82
#腹膜假黏液瘤#
81
#黏液瘤#
97
#生存率#
0
#腹膜#
71
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
129