Signal Transduct Target Ther:浙大蔡秀军团队揭示外泌体介导的肝癌靶向耐药细胞间传播新机制
2020-12-31 BW Bio生物世界
肝细胞癌(HCC)是最常见的原发性肝癌,在全球范围内,其发病率位于恶性肿瘤的第六位,其病死率在肿瘤相关死亡原因中的排名第四。对于晚期肝癌,索拉非尼是首个获得FDA批准的靶向治疗肝细胞肝癌的药物。
肝细胞癌(HCC)是最常见的原发性肝癌,在全球范围内,其发病率位于恶性肿瘤的第六位,其病死率在肿瘤相关死亡原因中的排名第四。对于晚期肝癌,索拉非尼是首个获得FDA批准的靶向治疗肝细胞肝癌的药物,既往研究表明,索拉非尼可以有效延长晚期肝细胞肝癌患者的中位总生存期。但是,往往在治疗6个月后,许多肝细胞肝癌患者会发生索拉非尼耐药,进而出现进展和转移,使下一步治疗变得非常棘手。
近日,浙江大学医学院附属邵逸夫医院蔡秀军教授团队在肝癌靶向治疗耐药领域获突破性进展,在Nature出版集团旗下权威学术期刊 Signal Transduction and Targeted Therapy(IF=13.493)上发表了题为:CircRNA-SORE mediates sorafenib resistance in hepatocellular carcinoma by stabilizing YBX1 的研究。
该研究阐明了 circRNA-SORE 在肝癌索拉非尼耐药中的重要作用和作用机制。
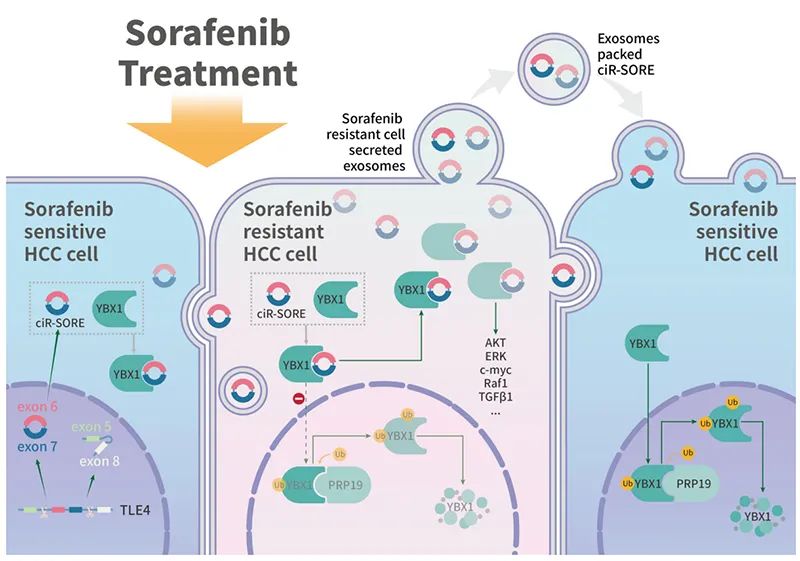
图1. 机制阐述
研究团队发现circRNA-SORE表达水平在耐药肝细胞肝癌细胞株中显著升高,而抑制其表达可以显著增强索拉非尼对肿瘤细胞的杀伤作用。
进一步研究发现,circRNA-SORE通过结合YBX1蛋白,将其相对稳定在细胞质中,从而减少YBX1在细胞核中由PRP19介导的泛素化降解。更重要的是,研究团队发现circRNA-SORE可以通过外泌体在细胞间传播,介导非耐药细胞获得耐药性。这一发现不仅为肝细胞肝癌靶向治疗耐药的干预靶点提供了理论依据,更提供了预判耐药人群较稳定的生物标志物,有望在今后的临床实践中得到更广泛的应用。
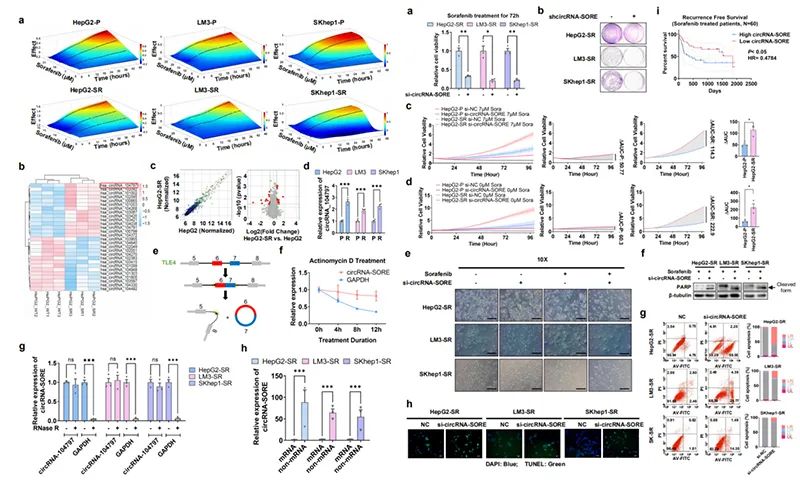
图2. circRNA-SORE在索拉非尼耐药的肝细胞肝癌中明显升高,并且在耐药的发生中发挥重要意义
研究团队首先建立了索拉非尼耐药的肝癌细胞系,并通过circRNA芯片、后续鉴定分析锁定了在耐药株中高表达且扮演重要角色的circRNA_104797,并将其命名为circRNA-SORE。
让研究小组眼前一亮的是,无论从细胞形态、细胞凋亡、细胞数量、细胞活力还是克隆形成能力来看,敲减circRNA-SORE均可极大程度地增加索拉非尼对肝细胞肝癌的抑制作用,而这种“增敏效应”在耐药细胞株中尤为突出,而野生细胞株却并不显著。

图3. circRNA-SORE通过结合YBX1,减少其在细胞核中被RPR19降解,而促进肝癌索拉非尼耐药
那么,如此重要的circRNA究竟通过什么机制参与了肝癌的索拉非尼耐药?
研究团队应用质谱技术鉴定了179种与circRNA-SORE特异性结合的蛋白,同时也分别鉴定了敲减circRNA-SORE 后129个上调蛋白和301个下调蛋白。综合分析两组质谱数据,研究团队发现YBX1蛋白与circRNA-SORE结合,且在敲减circRNA-SORE之后显著下调。
研究团队进一步挖掘了两者的结合位点,并采用突变表达、吗啉反义寡核苷酸阻断、共聚焦成像以及一系列免疫共沉淀试验得到验证。体外细胞实验和临床数据分析提示,circRNA-SORE可通过增加YBX1而促进耐药的形成,而敲减circRNA-SORE能显著增加YBX1的降解。
人体内蛋白质降解的途径有多种,比如溶酶体途径、泛素-蛋白酶体途径以及caspase(半胱天冬酶)降解途径。那么,一个环状RNA究竟是如何增加YBX1蛋白的降解呢?这个问题困扰研究团队许久,直到在敲减circRNA-SORE后与YBX1结合的蛋白谱发生了细微差异,研究团队敏锐地观察到了这一现象并设计严密的实验进行验证,答案逐渐浮出水面。在敲减circRNA-SORE时,PRP19与YBX1的作用增加,PRP19作为E3酶增加YBX1的泛素化,继而促进其降解。进一步研究惊喜地发现,主要位于胞质内的circRNA-SORE可以通过与YBX1相结合而降低YBX1的入核比例,进而减少YBX1被PRP19作用而降解。
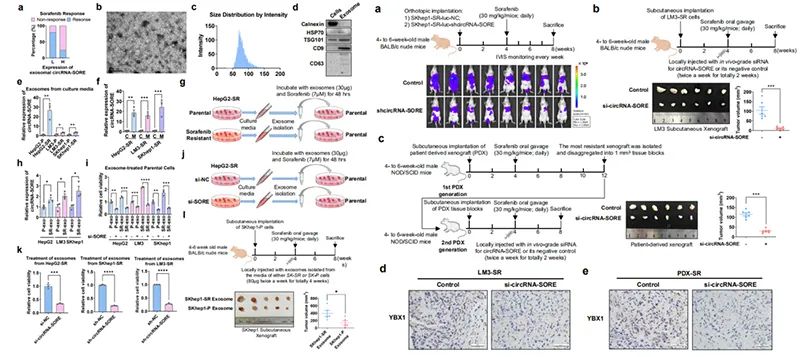
图4. 体内及体外实验发现circRNA-SORE可通过外泌体在细胞间传递索拉非尼耐药性,敲减circRNA-SORE可以显著使肝癌对索拉非尼增敏
肝癌是异质性非常强的恶性肿瘤,不同肿瘤细胞对药物的反应也不尽相同,肝癌靶向治疗耐药的过程也不会是一个同步的过程。首批获得耐药性的肿瘤细胞是否有可能将其耐药性通过细胞间沟通的方式(如外泌体)向敏感的肿瘤细胞传播而导致群体性耐药呢?带着这个猜想,研究团队尝试从使用索拉非尼的临床患者血清外泌体中寻找答案。
结果显示,对索拉非尼应答较差的患者在血清外泌体中存在更高水平的circRNA-SORE。体外细胞实验进一步证实,耐药细胞分泌的外泌体中含有比野生细胞更多的circRNA-SORE,在高表达circRNA-SORE外泌体的治疗下,野生细胞中的circRNA-SORE水平增加且耐药性也获同步增加,这一发现也得到小鼠动物实验的验证。
最后,研究团队构建了CDX和PDX小鼠索拉非尼耐药模型,验证了前述的研究发现,证实了敲减circRNA-SORE可增加索拉非尼对肿瘤的抑制并降低YBX1 的水平。
该成果的3点重要创新发现:
(1)首次鉴定了在肝癌索拉非尼耐药中具有关键作用的circRNA-SORE;
(2)首次揭示了PRP19对YBX1的促泛素化和降解作用;
(3)首次发现外泌体-circRNA-SORE介导的肝癌索拉非尼耐药性的细胞间传播。
综上,研究团队发现circRNA-SORE在索拉非尼耐药形成过程中发挥了重要的作用。本研究设计严谨、思路新颖,为肝细胞肝癌的临床诊疗提供了新的思路。蔡秀军教授是论文的通讯作者,徐俊杰博士后为论文的第一作者。该项研究受到国家重大科研项目、国家自然科学基金项目、浙江省重点研发计划、中国博士后科学基金项目等资助。
原始出处:
Junjie Xu , Lin Ji, Yuelong Liang,et al.CircRNA-SORE mediates sorafenib resistance in hepatocellular carcinoma by stabilizing YBX1. Signal Transduct Target Ther. 2020 Dec 26;5(1):298. doi: 10.1038/s41392-020-00375-5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Sign#
0
#target#
112
#TRA#
118
#Signal#
111
#浙大#
107
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
127
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
133