EUR HEART J:5年的临床和超声心动图的研究结果表明经导管主动脉瓣移植(TAVI)自我扩张型人工瓣膜可用于治疗严重的主动脉瓣狭窄!
2017-06-14 MedSci MedSci原创
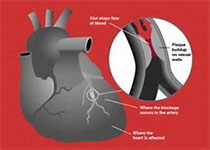
在现实生活中,有症状且主动脉瓣高度狭窄的患者进行瓣膜置换术手术风险很高,该研究的目的是评估经导管主动脉瓣移植(TAVI)自我扩张型人工瓣膜的安全性和有效性。
在现实生活中,有症状且主动脉瓣高度狭窄的患者进行瓣膜置换术手术风险很高,该研究的目的是评估经导管主动脉瓣移植(TAVI)自我扩张型人工瓣膜的安全性和有效性。
研究参与者来自12个国家44个有经验的中心。患者的资格、治疗方法和麻醉的选择是由当地的心脏小组决定的。该研究是100%的监测,并且不良事件由独立的临床事件委员会通过使用瓣膜学术研究协会(VARC-1)的标准来评定。
共有1015名患者参加了996次经导管主动脉瓣移植(TAVI)手术。平均年龄为81岁,平均EuroSCORE评分为19.3±12.3%.。对465名(46.7%)患者进行了5年随访。5年中,全因死亡率为50.7%(95%置信区间:46.7%,54.5%),主要中风率为5.4%。对配对的患者来说,血液动力学指标保持一致,其平均主动脉瓣梯度为8.8±4.4mmHg (n=198) ,有效的节流孔口面积为1.7±0.4cm2 (n=123)。
主动脉瓣反流(AR)随着时间的推移而减少,在5年(n=125)中,配对的患者的中度主动脉瓣反流从12.8%下降到8.0%。在860名患者的超声心动图数据或30天后再干预治疗中,有22名(2.6%)患者符合VARC-2标准的瓣膜功能障碍,10名(1.2%)患者在30天后再次干预。
结论
5年的研究结果表明,年龄较大、高风险的患者在接受了自我扩张型人工瓣膜植入术后有较低的再干预和血液动力学瓣膜功能障碍,为持久的瓣膜耐用性提供了证据。
原始出处:
Ulrich Gerckens,Corrado Tamburino,Sabine Bleiziffer,et al. Final 5-year clinical and echocardiographic results for treatment of severe aortic stenosis with a self-expanding bioprosthesis from the ADVANCE Study. European Heart Journal. 2017 June.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#研究结果#
54
#人工瓣膜#
80
#扩张#
63
#心动图#
0
继续努力
109
学习了,谢谢分享
117
好文章学习了
136
#经导管#
85
#HEART#
48
#主动脉#
56