Oncotarget: 细胞松弛素B诱导的膜囊泡表达亲代细胞的血管生成活动
2017-08-22 MedSci MedSci原创
喀山联邦大学基础医学和生物学研究所的Albert Rizvanov教授领导的研究团队已经证明,由细胞松弛素B治疗人类细胞所产生的人工膜囊泡能够保留血管生成活性。囊泡是从细胞释放的物质,它可以将物质和信息传送到邻近和远处的细胞。小泡是正常生理的重要调节因子,也与疾病有关,尤其是癌症。胞外囊泡表现出其亲本细胞的生物活性。例如,干细胞的胞外囊泡能促进血管生成和再生。因此,细胞外囊泡是一种有前景的传递生物
喀山联邦大学基础医学和生物学研究所的Albert Rizvanov教授领导的研究团队已经证明,由细胞松弛素B治疗人类细胞所产生的人工膜囊泡能够保留血管生成活性。
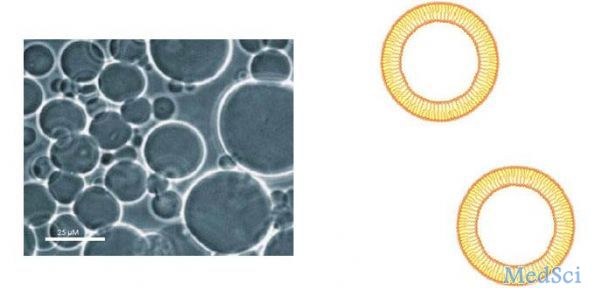
囊泡是从细胞释放的物质,它可以将物质和信息传送到邻近和远处的细胞。小泡是正常生理的重要调节因子,也与疾病有关,尤其是癌症。胞外囊泡表现出其亲本细胞的生物活性。例如,干细胞的胞外囊泡能促进血管生成和再生。因此,细胞外囊泡是一种有前景的传递生物活性分子的无细胞治疗方法。
然而,天然囊泡的产率太低,无法达到实际的目的。最近,有几项研究证明,在细胞中加入药物,细胞松弛素B,可使细胞产生膜囊泡的能力大大增加。这种方法在产生大量的细胞外囊泡的同时可以节约成本。然而,这些细胞松弛素B诱导的微囊泡(CIMV)是否保留了其亲本细胞的特征性生物学特性尚不清楚。
为了解决这一问题,由俄罗斯喀山联邦大学(Kazan Federal University)教授阿尔伯特·里兹瓦诺夫(Albert Rizvanov)和国际合作者组成的一个国际研究小组,对膜泡的生物活性进行了测定。
这项研究发表在《Oncotarget》杂志上。文章作者Marina Gomzikova博士和他的同事们描述了细胞松弛素B诱导的膜囊泡(CIMVs)的形态学、分子组成、融合能力和生物学活性。这些数据表明,CIMVs的生物物理、分子和大小分布特性与天然囊泡相似。此外,他们还证明了CIMVs保留了供体细胞的生物学特性,因为它们可以刺激体外和体内的血管生成。
现在可以大批量生产CIMVs,并将其规模扩大到工业生产水平; 目前有可能为具有生物活性的CIMVs分子提供治疗潜在的治疗方法。
原文出处:Marina O. Gomzikova, Margarita N. Zhuravleva, Regina R. Miftakhova, et al. Cytochalasin B-induced membrane vesicles convey angiogenic activity of parental cells. Oncotarget.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞松弛素#
30
#target#
32
#囊泡#
37
学习了谢谢分享
48