JAMA Netw Open:小儿2型糖尿病高血压和蛋白尿的患病率
2021-05-02 MedSci原创 MedSci原创
在这项研究中,儿童2型糖尿病的高血压和蛋白尿负担非常大,特别是在太平洋岛民和土著青年中。

Pixabay.com
全球肥胖人数的增加导致儿童出现2型糖尿病的风险增加。儿童2型糖尿病是一种侵袭性疾病,与儿童1型糖尿病或成人2型糖尿病相比,终末器官损害和合并症的风险更大。
适当的血糖和血压控制可以延缓终末期肾病的发生,降低微血管和大血管并发症的风险,使高血压和蛋白尿的管理成为改善儿童2型糖尿病患者预后的关键。然而,2型糖尿病患儿糖尿病相关肾病的全部负担尚未确定。还有一些证据表明,2型糖尿病并发症的发生率因性别和种族/民族而异。确定性别、种族/民族与高血压和蛋白尿患病率的关系是识别高危人群的重要一步,可以为未来的个性化筛查和治疗策略提供信息。
基于此,有研究者总结了2型糖尿病患儿中高血压和蛋白尿的患病率,并探讨性别和种族/民族与患病率的关系,以供临床医生作为参考,该研究结果近日发表在JAMA Netw Open期刊上。
从数据库建立之日起至2020年2月20日,对MEDLINE、Embase、CINAHL、Cochrane图书馆、科学网、灰色文献和筛选文章的参考文献进行搜索。
至少有10名参与者参与了2型糖尿病患儿高血压和/或蛋白尿患病率的观察研究。由两名独立评审员组成的三个小组筛选了7614篇论文,其中60篇符合资格标准。
主要结果包括高血压和蛋白尿的合并患病率(95% CI的百分比)。次要结果评估了按性别和种族/民族群体划分的综合流行率。
最后,系统评价包括60项研究。糖尿病病程从诊断时的纳入到诊断后的15.0年不等,报告的平均诊断年龄从6.5岁到21.0岁不等。3463名受试者高血压患病率为25.33%。男性参与者的高血压风险高于女性参与者,太平洋岛民和土著青年在所有种族/族裔群体中的患病率最高(太平洋岛民青年:26.71%;土著青年:26.48%;白人青年:20.95%;非裔美国青年:19.04%;拉美裔/拉丁美洲青年:15.11%;亚洲青年:18.37%。2250名受试者的蛋白尿患病率为22.17%(95%CI,17.34%-27.38%)。太平洋岛民青年、土著青年和亚洲青年的患病率高于白人青年(太平洋岛民青年:31.84%;土著青年:24.27%;亚洲青年:23.00%;白人青年:12.59%,无性别差异(或男性与女性参与者,0.68[95%CI,0.46-1.01])。研究的异质性很高,偏倚的风险从低到中等。
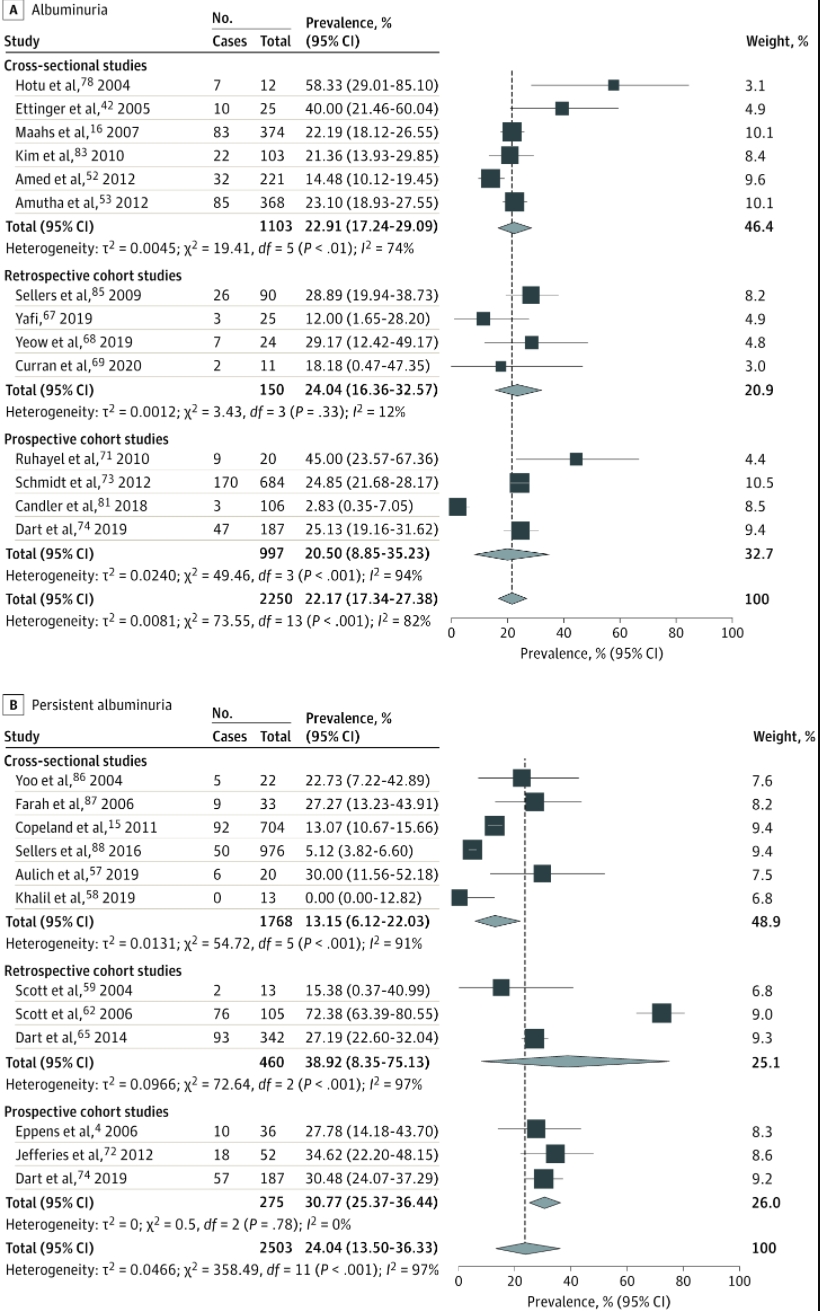
儿童2型糖尿病中蛋白尿和持续蛋白尿合并流行的森林图
此外,这篇综述还表明1/5到1/4的2型糖尿病患儿有蛋白尿。虽然未发现性别差异,但太平洋岛民、土著和亚洲青年的蛋白尿率高于白人青年。虽然有4%的受试者出现大量蛋白尿,但很少有研究报告持续性蛋白尿,需要进一步确认持续性蛋白尿是诊断蛋白尿的关键标准。
总之,在这项研究中,高血压和蛋白尿是儿童2型糖尿病的常见合并症,太平洋岛民和土著青年在这些疾病上的负担比其他种族的青年高得不成比例。目前迫切需要个性化筛选和治疗策略,以预防终末期肾脏疾病和心血管疾病的发生发展,并提高预期寿命。
参考文献:Cioana M, Deng J, Hou M, et al. Prevalence of Hypertension and Albuminuria in Pediatric Type 2 Diabetes: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(4):e216069. doi:10.1001/jamanetworkopen.2021.6069
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NET#
69
#PE#
66
#糖尿病高血压#
71
#患病率#
68
学习
104
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
83
谢谢MedSci提供最新的资讯
76
学习了,涨知识了!
90
哦哦
91
了解
60