Acta Anaesthesiol Scand:论如何改善肥胖手术患者的氧和作用
2015-08-30 MedSci MedSci原创
对肥胖患者来说,麻醉诱导的肺不张以及气道闭塞现象是很常见的,而肺不张和气道阻塞引起的静脉血掺杂,可影响肺通气血流比值,并进而阻碍全麻期间机体的氧合作用。近期,瑞典乌普萨拉大学的研究人员,对预充氧期间使用持续气道正压通气(CPAP)以及在麻醉苏醒期降低吸入氧浓度(FI02),是否可以提高进行腹腔镜手术的肥胖患者的氧合作用进行了探讨。 本次研究将患者随机分为2组:干预组(n=20,
对肥胖患者来说,麻醉诱导的肺不张以及气道闭塞现象是很常见的,而肺不张和气道阻塞引起的静脉血掺杂,可影响肺通气血流比值,并进而阻碍全麻期间机体的氧合作用。近期,瑞典乌普萨拉大学的研究人员,对预充氧期间使用持续气道正压通气(CPAP)以及在麻醉苏醒期降低吸入氧浓度(FI02),是否可以提高进行腹腔镜手术的肥胖患者的氧合作用进行了探讨。
本次研究将患者随机分为2组:干预组(n=20, 平均 BMI为 41.9),在预充氧以及麻醉诱导期间使用10cmH2O的持续气道正压通气;对照组(n=20, 平均BMI为38.1),在预充氧以及麻醉诱导期间未使用持续气道正压通气。在麻醉期间,所有患者使用容量控制模式进行通气:吸入氧浓度为0.4,呼气末正压通气(PEEP)为10 cmH2O。麻醉苏醒期:在拔管前,给予控制组患者的吸入氧浓度为1.0,并进一步将干预组分为2个小组,给与患者的吸入氧浓度分别为1.0和0.31。通过估算静脉血掺杂(EVA)对患者围术期氧合作用进行评估。
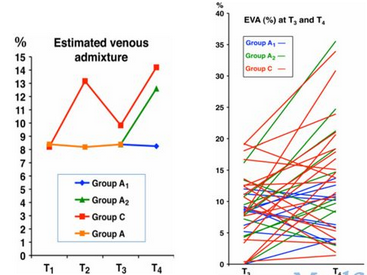
结果显示,在预充氧前两组患者的平均EVA大约为8%。麻醉插管后,干预组患者的平均EVA为8.2%,控制组患者的平均EVA为13.2% (P = 0.048)。在进行二氧化碳气腹后,干预组患者的平均EVA为8.4%,控制组患者的平均EVA为9.9% (P>0.05)。在术后一小时内,吸入氧浓度为1.0的患者在苏醒期出现氧合作用的恶化,而吸入氧浓度为0.31的患者的氧合作用则没有出现下降的现象。
本研究表明:在预充氧和麻醉诱导期对患者进行持续气道正压通气(10cmH2O),随后在插管后进行呼气末正压通气,似乎可以有效维持患者麻醉期间的氧合作用;而患者术后的氧合作用则取决于麻醉苏醒期的吸入氧浓度。
原始出处:
L.Edmark1, E.Ostberg1 et al.Preserved oxygenation in obese patients receiving protective ventilation during laparoscopic surgery:a randomized controlled study. Acta Anaesthesiol Scand. 2015 Aug 3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










文章不错,值得拜读
56
值得看,好好收藏,谢谢分享
126
#ANA#
39
#CTA#
39
#EST#
41
#ESI#
38