Clin Cancer Res:III期临床研究NALA(来那替尼+卡培他滨 vs 拉帕替尼+卡培他滨)的标志物探索
2021-09-23 yd2015 MedSci原创
该研究表明,PIK3CA突变预示更差的PFS,而高HER2表达水平预示更长的PFS。对比拉帕替尼+卡培他滨(LC),高HER2表达水平预示更能从那替尼+卡培他滨(NC)治疗获益。
NALA (NCT01808573)是一项随机、国际、多中心的III期临床研究,评估在经治的转移性HER2阳性乳腺癌患者中,来那替尼+卡培他滨(N+C)对比拉帕替尼+卡培他滨(L+C)的疗效和安全性。研究表明来那替尼+卡培他滨(N+C)较拉帕替尼+卡培他滨(L+C)改善经治的HER2阳性转移性乳腺癌(MBC)患者的无进展生存期(PFS)。近期,研究团队对NALA研究进行标志物探索。研究成果发表在Clin Cancer Res杂志上。
621例HER2阳性MBC患者随机分配到NC或LC组。大多数样本来自原发肿瘤(n=393;63%),其余为转移性(n=184;30%)或其他无特征的(n=63)。在621个可用样本中,420名患者(68%)进行了NGS检测, 615名(99%)患者进行HER2 IHC染色进行H-scoring,526名患者(85%)报告了HERmark评分,451名患者(73%)报告了VeraTag p95评分。
420例患者 进行NGS测序,常见的体细胞突变为PIK3CA 34%(143/420); HER2 5% (23/420); HER3 1%(4/420), AKT1 1% (3/420),和ESR1 2%(7/420)。
PIK3CA 突变患者的PFS较野生型患者有缩短的趋势,跟治疗手段无关,PFS分别为5.55和 4.34个月(HR=0.81,95% CI, 0.64–1.03)。HER2野生型患者PFS为5.45个月, HER2突变型患者PFS为5.72个月[HR=1.686,95% CI, 0.967-3.288)。HER2突变不能预测NC对比LC的PFS获益(P=0.502)。在多变量Cox模型中调整其他预后因素后,PIK3CA突变患者跟更短PFS相关的趋势[HR=0.82,95% CI, 0.65-1.05]。同样,PIK3CA突变也不能预测NC对比LC的PFS获益(P=0.995)。

PIK3CA和HER2状态PFS
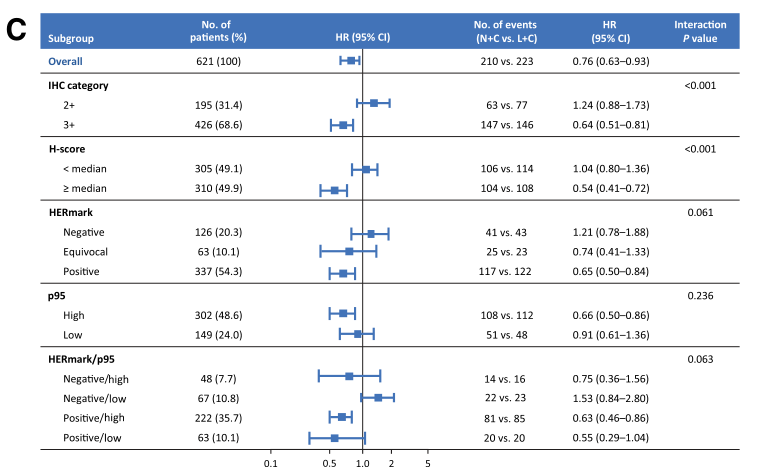
高HER2蛋白水平是跟更长的PFS相关[IHC 3+ vs. 2+,HR=0.67 (0.54–0.82); H-score ≥240 vs <240, HR=0.77 (0.63–0.93); HERmark positive vs.negative,HR=0.76,(0.59–0.98)]。

较高的p95与PFS受益更倾向于NC而非LC组[高p95 (≥2.8 RF/ mm2): HR=0.66 (95% CI, 0.50 0.86) vs低p95 (<2.8 RF/ mm2): HR=0.91 (95% CI, 0.61 1.36);p=0.236]。NC vs LC 获益倾向的是HERmark-positive/p95-high [HR= 0.63 (95% CI, 0.46–0.86)],还有HERmark-positive/p95-low [HR =0.55 (95% CI, 0.29–1.04)](P=0.063)。
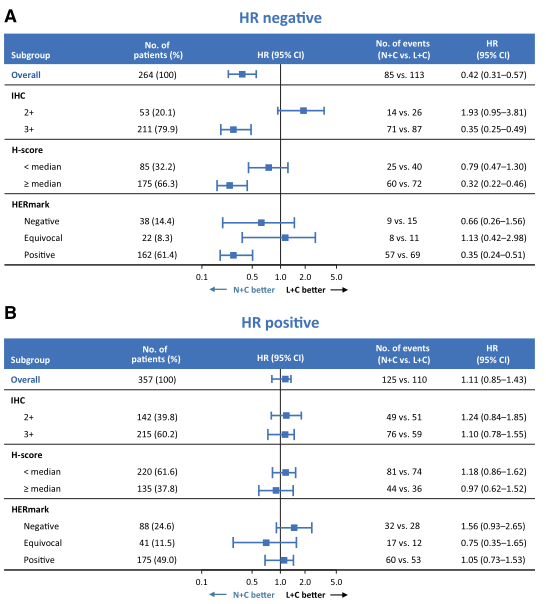
HR阴性患者,NC较LC可获得PFS获益[HR=0.42(95% CI, 0.31–0.57)],而在HR阳性患者,两组没有统计学差异[HR=1.08 (95% CI, 0.84–1.40)]。HR-/HER2+患者,NC对比LC组的PFS获益更明显[IHC 3+: HR=0.35 (95% CI, 0.25–0.49); H-score ≥240: HR=0.32 (95% CI, 0.22–0.46); HER-mark-positive: HR=0.35 (95% CI, 0.24–0.51)]。
综上,该研究表明,PIK3CA突变预示更差的PFS,而高HER2表达水平预示更长的PFS。对比拉帕替尼+卡培他滨(LC),高HER2表达水平预示更能从那替尼+卡培他滨(NC)治疗获益。
原始出处:
Saura C, Matito J, Oliveira M, et al. Biomarker Analysis of the Phase III NALA Study of Neratinib + Capecitabine vs Lapatinib + Capecitabine in Patients with Previously Treated Metastatic Breast Cancer. Clin Cancer Res. 2021 Aug 11:clincanres.1584.2021. doi: 10.1158/1078-0432.CCR-21-1584. Epub ahead of print. PMID: 34380637.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#III#
67
#III期临床研究#
103
#II期临床研究#
61
#标志物#
64
#I期临床#
77
#ALA#
74
#卡培他滨#
69
#拉帕替尼#
72
#II期临床#
72
#III期#
72