Blood:纳米单抗Caplacizumab实际应用于TTP患者的真实临床数据
2020-11-17 MedSci原创 MedSci原创
血浆交换(PEX)联合免疫调节策略是免疫介导性血小板减少性紫癜(iTTP)挽救生命治疗的基础。Caplacizumab是一种新型的抗von Willebrand因子纳米体,两个多中心、随机的、安慰剂对
血浆交换(PEX)联合免疫调节策略是免疫介导性血小板减少性紫癜(iTTP)挽救生命治疗的基础。Caplacizumab是一种新型的抗von Willebrand因子纳米体,两个多中心、随机的、安慰剂对照的临床试验的结果使其获得了EU和FDA的批准,已通过患者准入计划在英国(UK)上市。
Tina等人从22家UK医院回顾性地收集了于2018年-2020年接受Caplacizumab治疗的85位患者的数据,包括4名儿童。将实际临床应用中的患者特征和预后与Caplacizumab临床试验的终点和Caplacizumab前时代的历史性预后进行对比。
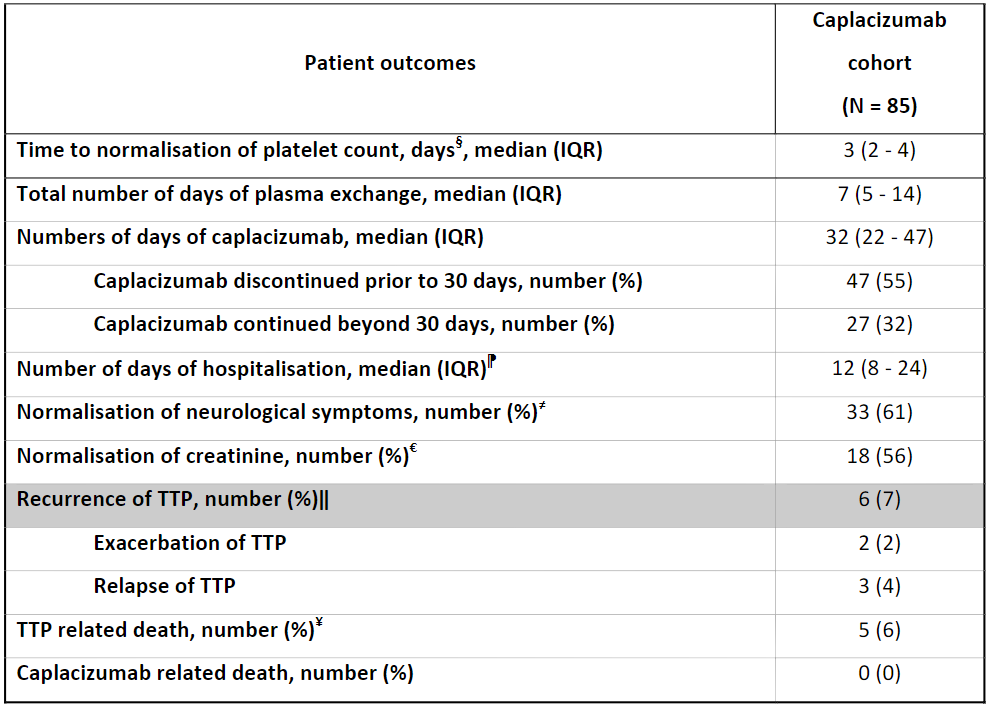
TTP患者接受Caplacizumab治疗的预后汇总
84位患者在进行PEX的同时还使用了类固醇和利妥昔单抗;26%的患者需要插管。血小板恢复计数正常的中位时间(3天)、PEX中位持续时间(7天)和中位住院时间(12天)均与RCT数据相当。PEX的中位持续时间和从开始PEX到血小板计数正常的时间均优于历史预后(p<0.05)。5位患者的TTP复发;这5位患者的ADAMTS13活性持续低于5iu/dL。26位患者共发生了31例不良反应事件,其中17例(55%)是出血、5例(16%)是血栓性事件(两例与Caplacizumab无关)。死亡率为6%(5/85),无死亡病例归因于Caplacizumab;在4例死亡病例中,Caplacizumab是在PEX开始48小时后才开始应用(3-21天)。
这些数据是在临床试验之外,Caplacizumab在临床实践中实际应用于TTP患者的第一批也是最大量的数据,包括儿科患者。该结果代表了真正的临床实践,为全球的临床医生治疗TTP提供了宝贵的经验。
原始出处:
Dutt Tina,Shaw Rebecca J,Stubbs Matthew James et al. Real-World Evidence of Caplacizumab Use in the Management of Acute TTP. Blood, 2020, undefined: undefined.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#mAb#
64
#CAP#
76
什么时候来中国
66
#Caplacizumab#
0
#临床数据#
82
#TTP#
59
#APL#
65
好文章,谢谢分享
95