Nat Commun:社会我肠道菌!可通过改变细胞基因预防感染和癌症!
2018-01-22 佚名 生物探索
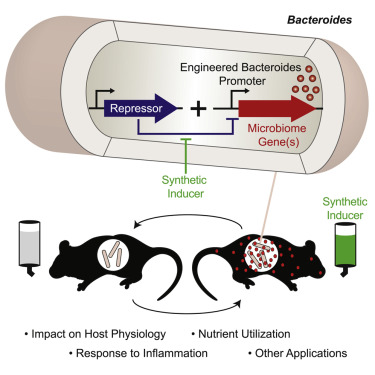
这项发表在Nature Communications杂志上的研究称,来自细菌的化学信息能够改变“整个人类基因组中的关键化学标记”。通过这种“交流”方式,肠道细菌可以帮助对抗感染及预防癌症。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#COMMUN#
101
#Nat#
102
#肠道菌#
73
#社会#
95
阅
139
学习了.涨知识
119
阅
105