JCEM:妊娠期TSH和FT4参考区间
2022-08-11 从医路漫漫 MedSci原创
建议使用特定于人群和三个月的TSH和FT4参考间隔作为黄金标准,在没有已知甲状腺疾病、最佳碘状况和甲状腺过氧化物酶抗体(TPOAb)状态为的人群中计算。
背景:妊娠期充足的甲状腺激素供应对于无并发症的妊娠以及最佳的胎儿生长和发育是重要的。妊娠期间甲状腺功能测试异常与不良妊娠和儿童结局的风险较高相关。然而,由于孕妇生理的变化,识别怀孕期间的甲状腺功能异常是复杂的。此外,由于不同的化验方法以及人群特征之间的显著差异,妊娠期TSH或FT4没有普遍的参考区间。国际甲状腺或内分泌学会目前的指南,包括美国甲状腺协会(ATA)最新的2017年指南,建议使用特定于人群和三个月的TSH和FT4参考间隔作为黄金标准,在没有已知甲状腺疾病、最佳碘状况和甲状腺过氧化物酶抗体(TPOAb)状态为的人群中计算。然而,对于许多实验室来说,这些都是不可用的,因为根据当地参考人群计算参考间隔通常是不可行的。ATA指南中最近提供的另一种选择是,要么将TSH的上限固定为4.0mU/L,要么在妊娠4个月的非妊娠参考上限中减去0.5mU/L。
ATA指南的最新补充是采用参考区间的选项,该参考区间是在具有相似人群的中心计算的,使用相同的检测方法,这是介于黄金标准和固定TSH上限方法之间的一步。然而,由于缺乏关于甲状腺激素参考区间的所有已发表数据的概述,确定可采用的TSH和FT4参考区间是困难的。此外,由于新的见解和不断变化的指南,研究之间存在着巨大的方法差异。其中一个例子是在当前ATA指南推荐的标准之外使用额外的排除标准,其中大多数仍然具有未知的意义,如甲状腺球蛋白抗体(TgAb)阳性、体外受精(IVF)受孕、妊娠并发症和特征,包括既往存在的糖尿病、高血压、异常体重指数(BMI)和经常吸烟。尽管这些因素中的一些是TSH和FT4浓度的决定因素,但只有一些但不是所有的研究表明,根据这些决定因素排除女性会影响TSH和FT4参考区间。研究之间方法差异的另一个例子是参考间隔的计算。一些研究用第5和第95个百分位数来定义参考区间,而在常规实验室实践中,通常使用第2.5到97.5个百分位数。虽然许多研究的方法与甲状腺或内分泌学会目前的国际指南不一致,但仍不清楚这在多大程度上影响计算的参考区间的概括性。
虽然与黄金标准相比,使用固定的TSH上限的方法可能会因为人群间和测定间的差异而导致相当大的低估和过度诊断,但从非妊娠参考区间减去绝对数的方法还没有得到彻底的研究。
目的:1)概述已发表的妊娠期TSH和FT4的参考区间;2)结合不同队列的原始数据,评估常见方法学研究间差异的后果。
方法:1)检索Ovid MEDLINE、EMBASE、Web of Science,检索至2021年12月12日。研究以一式两份进行评估。2)在甲状腺与妊娠联盟的参与队列中进行了个体参与者数据(IPD)荟萃分析。结果:1)研究间的方法学差异很大,102项纳入研究中有11项符合现行指南。2)纳入Meta分析的有22个队列,共63,198人。不排除TPOAb阳性的参与者导致所有队列中TSH上限的上升,特别是在第一个月(平均值:+17.4%[范围+1.6至+30.3%])和中期(平均值:+9.8%[范围[范围+0.6至+32.3%])。第95个百分位数的使用导致上限发生了很大变化,TSH从-10.8%到-21.8%,FT4从-1.2%到-13.2%不等。所有其他排除标准最多改变了3.5%的参考区间截止值。将这些发现应用于包括在系统综述中的102项研究,48项研究可以用于临床。
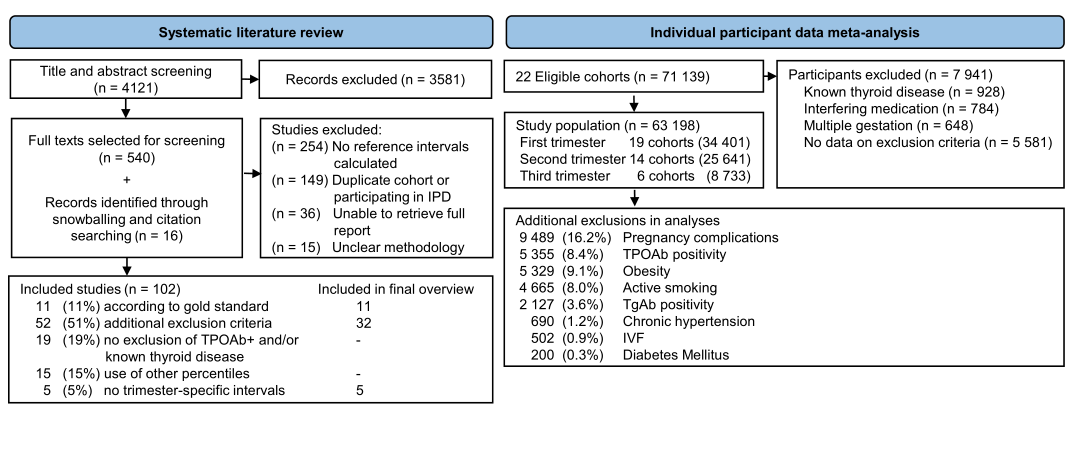
图1研究选择流程图。
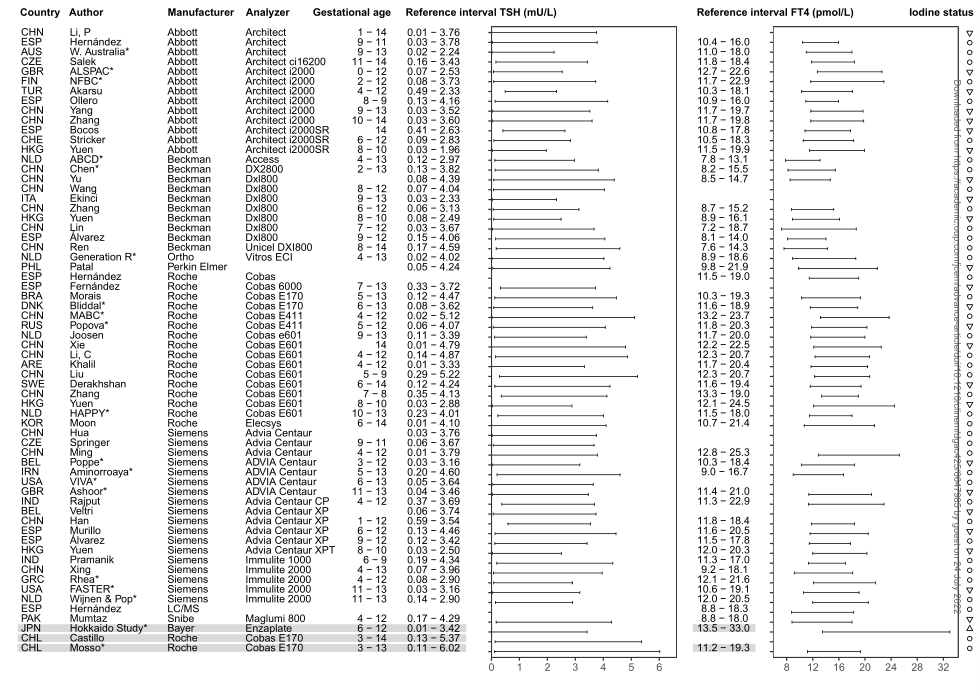
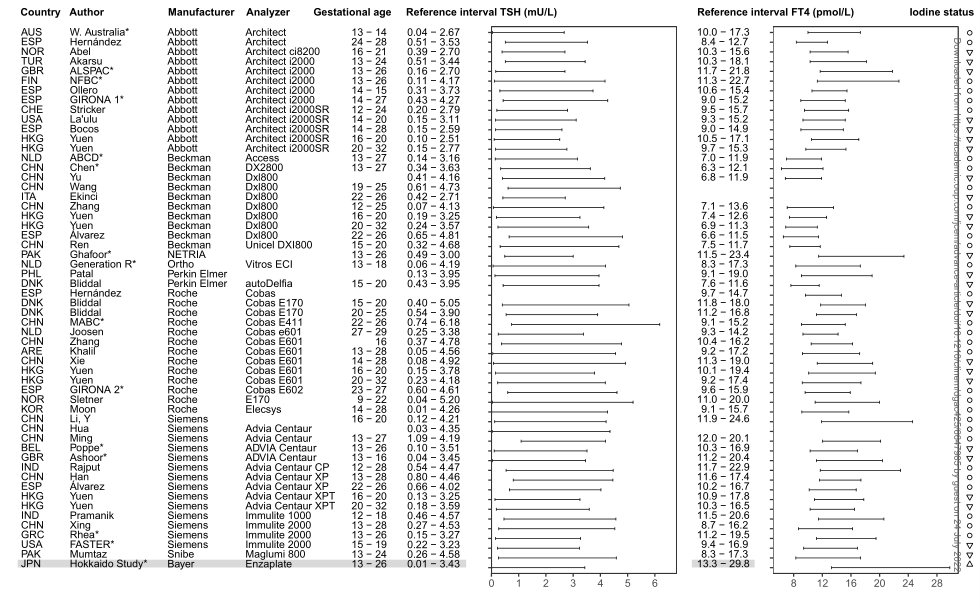
图2-3 *用联合体中个体参与者数据计算的参考区间;◯碘充足;▽轻中度碘缺乏;△碘过量状态。在碘状态波动或过量的队列中计算的参考区间以灰色列出。
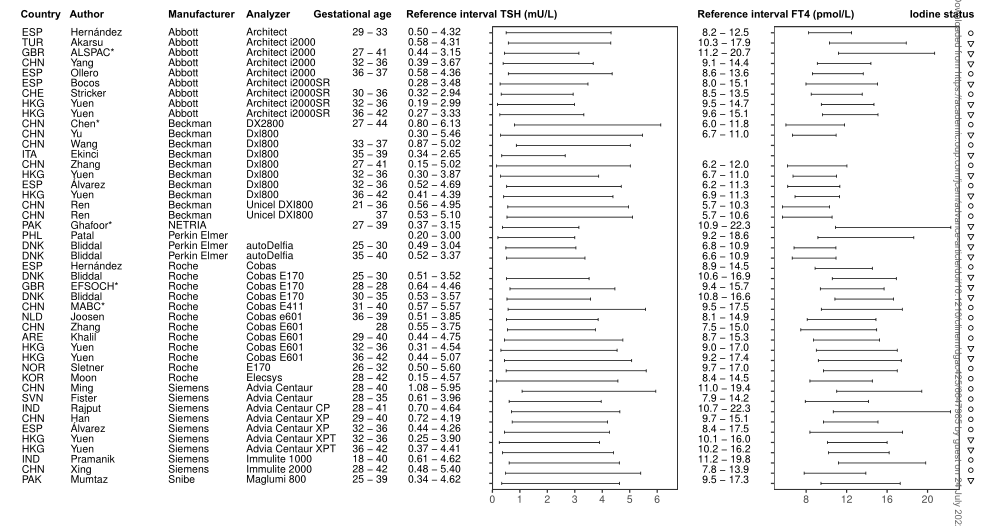
图4 *联合体中个体参与者数据计算的参考区间;◯碘充足;▽轻中度碘缺乏。
结论:我们提供了妊娠期TSH和FT4的临床相关参考区间的概述。Meta分析的结果表明,未来的研究可以采用简化的研究方案,而不需要额外的排除标准。
原文出处:Osinga JAJ, Derakhshan A, Palomaki GE,et al.TSH and FT4 reference intervals in pregnancy: a systematic review and individual participant data meta-analysis.J Clin Endocrinol Metab 2022 Jul 21
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
101
#JCEM#
70
#妊娠期#
80
#TSH#
98
#参考区间#
59