Nature:逆转糖尿病的革命性新成果
2019-02-14 佚名 生物通
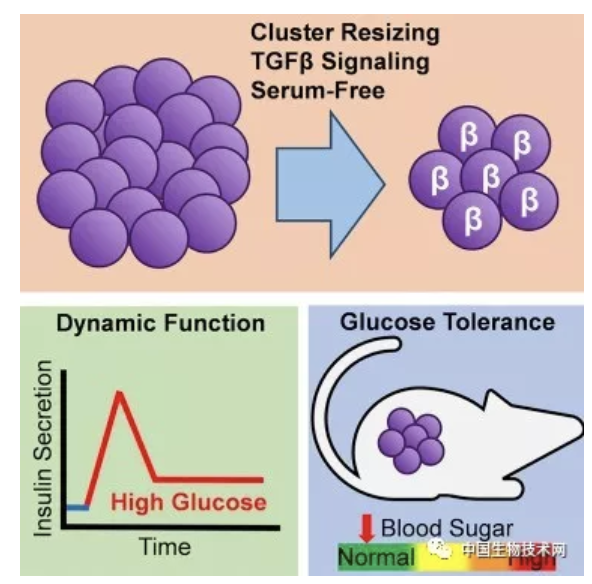
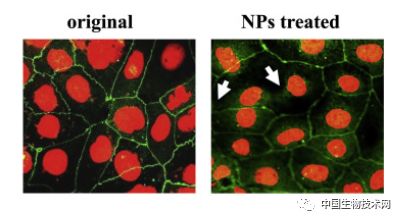
生物学教科书告诉我们:细胞分化后形成的成体细胞类型是固定的,但来自瑞士日内瓦大学(UNIGE)的一项最新研究第一次发现,不能产生胰岛素的人胰腺细胞可以通过诱导,改变自身功能,可持续的生成胰岛素,这表明我们细胞的适应能力远大于之前认为的。而且,这种可塑性不是人体胰腺细胞所独有的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新成果#
74
#Nat#
65
科研路漫漫,加油!
106
很好的资讯
99
谢谢MedSci提供最新的资讯
72