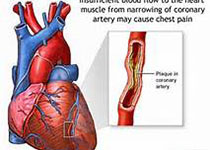
Circulation:ERV1/ChemR23信号可通过调节巨噬细胞氧化低密度脂蛋白的摄取和吞噬作用来预防动脉粥样硬化
2018-10-24 MedSci MedSci原创
血管炎症消退能力受损,除了会增强促炎信号,还在动脉粥样硬化中发挥重要作用。通过12/15脂氧合酶通路形成的促溶性脂质介质对小鼠动脉粥样硬化具有保护作用。n-3多不饱和脂肪酸,包括二十碳五烯酸(EPA),作为脂质介质形成的底物,可通过其同源G-蛋白偶联受体转化其潜在的抗炎和促溶作用。现研究人员对调节动脉粥样硬化疾病进展的EPA补充和脂质介质形成相关的信号通路进行研究。给Apoe-/-小鼠补充EPA后
血管炎症消退能力受损,除了会增强促炎信号,还在动脉粥样硬化中发挥重要作用。通过12/15脂氧合酶通路形成的促溶性脂质介质对小鼠动脉粥样硬化具有保护作用。n-3多不饱和脂肪酸,包括二十碳五烯酸(EPA),作为脂质介质形成的底物,可通过其同源G-蛋白偶联受体转化其潜在的抗炎和促溶作用。现研究人员对调节动脉粥样硬化疾病进展的EPA补充和脂质介质形成相关的信号通路进行研究。
给Apoe-/-小鼠补充EPA后进行脂浆分析,并建立Erv1/Chemr23-/-Apoe-/-小鼠模型,来评估动脉粥样硬化、吞噬作用和氧化低密度脂蛋白的摄取量。对人类动脉粥样硬化病灶进行组织学和mRNA分析。
研究人员发现EPA补充可显著延缓西式饮食诱导的Apoe-/-小鼠动脉粥样硬化病灶的生长。系统性的血浆脂质体分析显示消退素E1前体18单羟基EPA作为中心分子,在EPA补充时形成。在两种独立的高脂小鼠模型中,靶向敲除消退素E1受体Erv1/Chemr23与巨噬细胞中的促动脉粥样硬化信号、氧化低密度脂蛋白摄取增加、吞噬减少、动脉粥样硬化斑块大小增加和坏死核心形成有关。研究人员还发现在巨噬细胞中,消退素E1介导的氧化低密度脂蛋白摄取和吞噬作用依赖于Erv1/Chemr23。此外,研究人员在人动脉粥样硬化样本坏死核心附近的巨噬细胞中鉴定出了ERV1/ChemR23的表达,证实了他汀类药物使用者来源的斑块中ERV1/ChemR23的mRNA水平增加。
本研究明确了18-单羟基EPA是补充EPA后的主要血浆标志物,并证明了ERV1/ChemR23作为其下游介导物resolvin E1的受体在动脉粥样硬化中转导保护作用。ERV1/ChemR23信号或许可代表一种既往未被发现的可用于减少动脉粥样硬化性心血管疾病的治疗途径。
原始出处:
Andres Laguna-Fernandez,et al. ERV1/ChemR23 Signaling Protects Against Atherosclerosis by Modifying Oxidized Low-Density Lipoprotein Uptake and Phagocytosis in Macrophages. Circulation. July 21, 2018;138:1693–1705
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EMR#
111
#ChemR23#
70
#粥样硬化#
68
#吞噬作用#
86
#Erv1/Chemr23#
50
#脂蛋白#
75
冠状动脉硬化性心脏病的治疗。
98
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
113
学习了谢谢
121