尿检也能查CT/NG!NAATs技术保障女性生殖健康
2018-12-07 佚名 中国医学论坛报
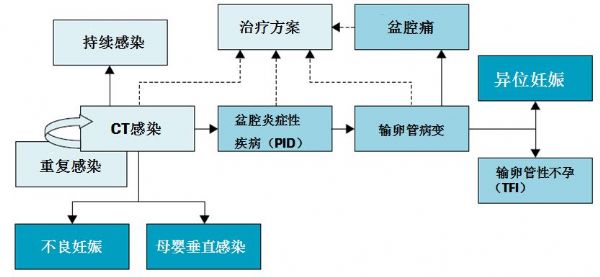
近日,在第十一届中华女性生殖道感染峰会“白云会”期间,清华长庚医院妇产科主任廖秦平教授、首都医科大学附属北京妇产医院妇科主任刘朝晖教授及中南大学湘雅三医院妇产科主任薛敏教授针对临床常见的沙眼衣原体(CT)、淋病奈瑟菌(NG)感染及其并发症防治问题展开了积极讨论。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#ATS#
80
#NAATs#
58
#女性生殖#
87
#尿检#
0
#生殖健康#
76
学习了长知识
92
学习了新知识
103
学习了长知识
103
学习了新知识
98
学习了长知识
111