Circulation:单细胞核RNA测序揭示扩张型心肌病儿科患者的分子特征
2021-05-02 Nebula MedSci原创
扩张型心肌病儿科患者的成纤维细胞和心肌细胞基因表达模式呈现显著的年龄依赖性的变化
扩张型心肌病(DCM)是心力衰竭儿童死亡的主要原因。小儿心力衰竭治疗的结果存在很大的异质性,并且缺乏大量的队列研究。可以通过考虑与年龄和疾病相关的病理生理学、病理学和分子指纹的个性化治疗来改善DCM患儿的治疗预后。
本研究旨在对DCM患儿进行单核RNA测序,以探究DCM的致病机制。
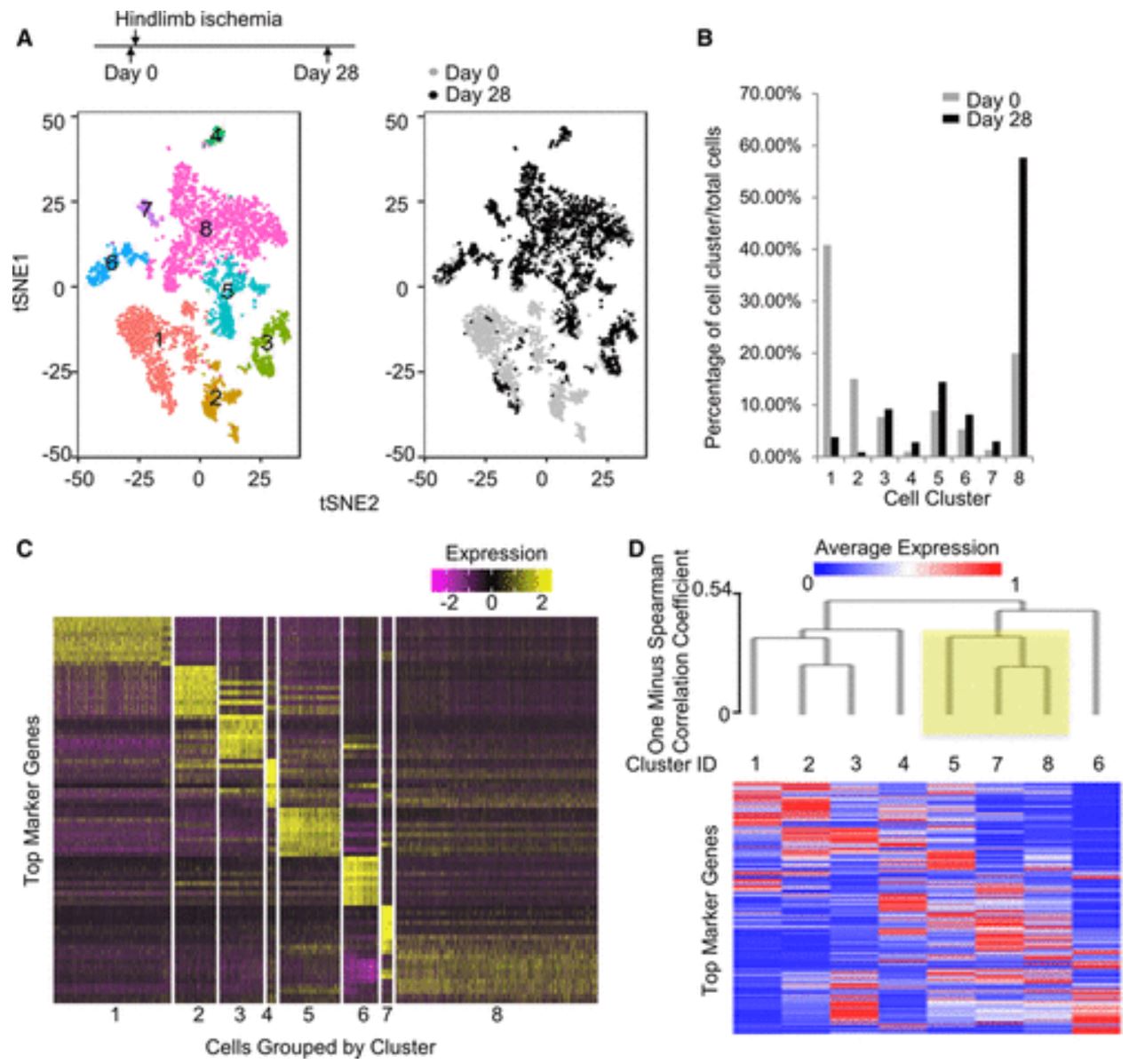
研究人员对6位DCM患儿(0.5岁、0.75岁、5岁、6岁、12岁和13岁)的心脏组织进行了单细胞核RNA测序。18211个细胞核的无监督聚类分析共鉴定出了具有6种主要细胞类型的14个不同簇。
不同年龄DCM患儿的心脏细胞核基因表达异质性
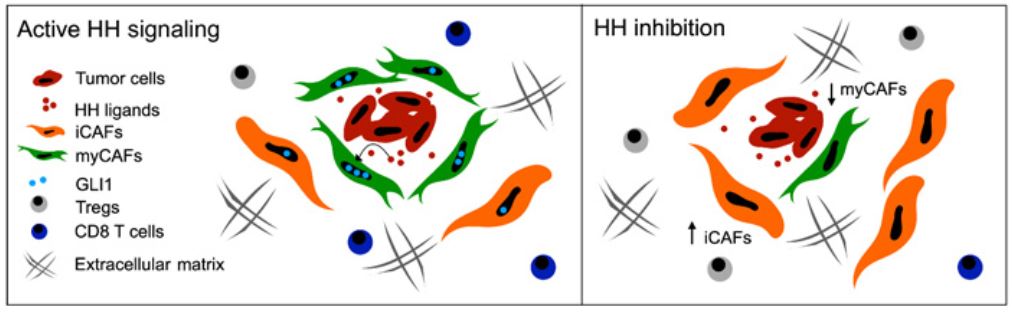
DCM患者成纤维细胞簇中的细胞核的数量随着年龄的增长而增加,组织学分析证实了这一发现,这一发现与通过心脏磁共振成像量化的与年龄相关的心脏纤维化增加相一致。6岁以上的DCM患者的成纤维细胞显示出明显改变的基因表达模式,其中编码原纤维胶原蛋白、调节蛋白聚糖、血小板反应蛋白同工型转换和成纤维细胞激活的基因显著富集。
DCM患儿心脏成纤维细胞数量呈年龄依赖性增加
此外,在DCM婴儿患者中还鉴定出了具有高再生特性的心肌细胞群,但在6岁以上的儿童中却没有。该簇显示了细胞周期激活因子(如小细胞周期蛋白D家族成员)的高表达、糖酵解代谢和抗氧化基因表达增加,以及β-肾上腺素能信号传导基因改变。
综上所述,本研究对DCM儿童患者心脏细胞转录组的分析揭示了成纤维细胞和心肌细胞基因表达模式的显著的年龄依赖性的变化;DCM婴儿患者的纤维化较少,促再生特征富集。
原始出处:
Luka Nicin, et al. Single Nuclei Sequencing Reveals Novel Insights Into the Regulation of Cellular Signatures in Children With Dilated Cardiomyopathy. Circulation. 2021;143:1704–1719
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#分子特征#
73
#儿科患者#
69
#扩张#
105
#RNA测序#
97
#细胞核#
99
#肌病#
72
好材料
92