NEJM:激素替代治疗可延缓早期绝经女性发生颈动脉粥样硬化
2016-04-03 徐媛 MedSci原创
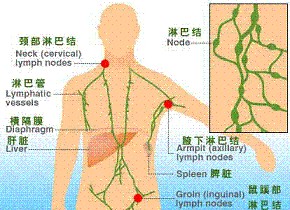
本研究旨在评估雌二醇(有或无孕激素)对颈动脉粥样硬化的影响。研究人员总共纳入643名健康的绝经女性,并根据更年期(< 6年[早期绝经后期]或≥10年[晚绝经后期])时间随机分配到两组中,一组给予17β-雌二醇1mg/日,另一组给予安慰剂。雌二醇组女性同时使用孕酮阴道凝胶,每日使用,连续10天,持续30天;安慰剂组女性以同样的用药方式使用安慰剂阴道凝胶。研究主要终点为6个月后测量女性的颈动脉内
本研究旨在评估雌二醇(有或无孕激素)对颈动脉粥样硬化的影响。研究人员总共纳入643名健康的绝经女性,并根据更年期(< 6年[早期绝经后期]或≥10年[晚绝经后期])时间随机分配到两组中,一组给予17β-雌二醇1mg/日,另一组给予安慰剂。雌二醇组女性同时使用孕酮阴道凝胶,每日使用,连续10天,持续30天;安慰剂组女性以同样的用药方式使用安慰剂阴道凝胶。研究主要终点为6个月后测量女性的颈动脉内膜中层厚度(CIMT),次要终点为通过心脏CT检查评估冠状动脉粥样硬化。
研究结果,中位随访时间平均为5年,不管是否使用黄体酮凝胶,绝经早期使用雌二醇组女性CIMT增加0.0044 mm/年,绝经早期使用安慰剂组为0.0078 mm/年(P =0.008);绝经晚期使用雌二醇组和绝经晚期使用安慰剂组参与者CIMT分别增加0.0100 mm/年和0.0088 mm/年(P =0.29)。雌二醇组和安慰剂组女性在心脏CT检查中的冠状动脉粥样硬化方面无显著差异。雌二醇组和安慰剂组女性的严重不良事件发生率相似。
研究结论,在早期绝经后期开始激素替代治疗(HRT)与晚绝经后期治疗相比可获益。绝经后期,雌二醇组和安慰剂组女性在心脏CT检查中冠状动脉粥样硬化方面无显著差异。
原始出处
Hodis HN1, Mack WJ1, Henderson VW1, Shoupe D1, Budoff MJ1, Hwang-Levine J1, Li Y1, Feng M1, Dustin L1, Kono N1, Stanczyk FZ1, Selzer RH1, Azen SP1; ELITE Research Group.Vascular Effects of Early versus Late Postmenopausal Treatment with Estradiol.N Engl J Med. 2016 Mar 31
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#替代治疗#
89
#颈动脉#
63
#粥样硬化#
84
#绝经女性#
66
#颈动脉粥样硬化#
79
#绝经#
67
谢谢分享。
110
希望有大样本的研究
153
和以前的研究结果不一致,还需要更多研究来评估
150
和以前的研究结果不一致,还需要更多研究来评估
153