Cancers:免疫相关甲状腺炎是转移性肾癌患者生存的预测因素
2022-03-08 从医路漫漫 MedSci原创
免疫治疗的广泛整合使癌症治疗发生了革命性的变化,同时引入了一类不同种类的免疫相关不良事件(IrAEs)。
背景:免疫治疗的广泛整合使癌症治疗发生了革命性的变化,同时引入了一类不同种类的免疫相关不良事件(IrAEs)。自2015年以来,检查点抑制剂(CPI)已被常规用于转移性肾细胞癌(MRCC)的治疗,最初是作为后续系列的单一疗法,目前处于一线环境,作为与血管内皮生长因子抑制剂(VEGFi)或第二CPI(nivolumab和ipilimumab)联合治疗的一部分。Heng等人提出的VEGFi时代mRCC患者的风险分层模型,根据总体生存(OS)对患者进行分层。该模型根据六个预后因素将患者分为有利风险组、中等风险组和不良风险组。这个临床模型已经在所有最近的免疫治疗III期试验中被用于风险分层,并预测了在中等风险到较低风险的患者中,免疫治疗组合相对于舒尼替尼的优越性。其他预测CPI反应的生物标志物仍在研究中。
目的:免疫检查点抑制剂(CPI)适用于转移性肾细胞癌(MRCC)。免疫相关甲状腺炎(IRT)是一种免疫相关不良事件(IRAE),影响高达30%的患者。我们的目标是确定IRT是否与mRCC的总体存活率相关。
方法:一项回顾性队列研究在2015年至2020年期间对在同一中心连续123名接受CPI治疗的肾细胞癌患者进行了研究。疾病风险分层通过两种方法进行评估:Heng标准和一种新的二分法分层系统,即“低风险”和“高风险”加上转移部位的数量。
结果:38%的患者发生了IRT。在一般队列中,IRT与生存益处无关。然而,根据Heng标准(n=17,HR=0.25,p=0.04)和新的“高危”组(HR=0.28,n=42,p=0.01),包括多因素分析中的协变量(HR=0.27,p=0.003),IRT与较好的生存相关(n=17,HR=0.25,p=0.04),而在新的“高危”组(HR=0.28,n=42,p=0.01)中,IRT与较好的生存相关。在整个队列或“高危”组中,无论是在整个队列中还是在“高危”组中,有任何IRAE都与提高整个队列的存活率有关,而与任何特定的IRAE没有显著的相关性。
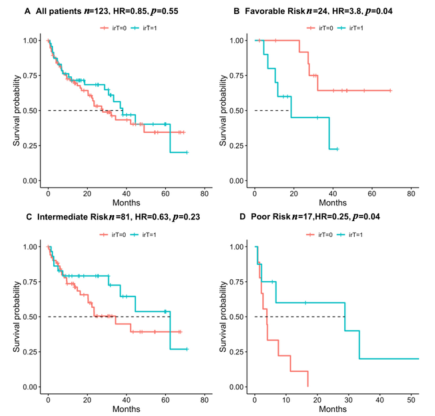
图1。所有患者和Heng危险组的IRT与生存期的关系。卡普兰-迈尔的总体生存情节。用Cox比例风险回归模型计算HR和P值

图2.新风险组的IRT与生存概率的关系。卡普兰-迈尔的总体生存情节。用Cox比例风险回归模型计算HR和P值。

表1.免疫相关不良事件在研究人群和高危人群中的患病率及其对生存的影响
结论:IRT是一种早期和普遍的IRAE,与较差/“高危”肾癌患者的生存时间延长有关。
原文出处:Sagie S, Gadot M, Levartovsky M, et al.Immune-Related Thyroiditis as a Predictor for Survival in Metastatic Renal Cell Carcinoma.Cancers (Basel) 2022 Feb 10;14(4)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







.jpg)




#患者生存#
125
#ERS#
86
#预测因素#
100
#转移性#
92
#甲状腺炎#
99