Lancet:剖宫产更佳手术方式5大困惑,你知道吗?
2016-05-09 Mechront&KL MedSci原创
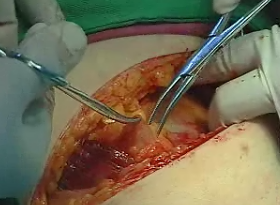
经阴道分娩是自然而且符合生理的分娩途径,产妇分娩后能迅速康复,新生儿能更好的适应外界环境。不过总是会有一些幺蛾子(包括医学指征和非医学指征)让女性不能顺利进行阴道分娩,这时候或许我们就需要经腹切开子宫取出胎儿,也就是剖宫产。 虽然在1610年进行了世界上第一例剖宫产,其产妇在术后25天死亡,不过到如今21世纪,数百年的发展已经让剖宫产变得安全可靠。产科医生进行一项普普通通没有并发症没

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#手术方式#
42
#Lancet#
40
值得一看
143
大家尽量顺其自然吧
121
挺好的
133
可以
131
而且剖宫产远期并发症此文并未提到
98
而且手术方式众多不一
101
希望患者认知有所提高
78
建议还是顺产好
81