Sci Rep:紧急避孕药和宫外孕风险之间的关系
2015-02-14 黄辛 科学网
国际学术刊物《科学报告》在线发表研究论文《左炔诺孕酮紧急避孕药与异位妊娠(宫外孕)风险:一项多中心病例对照研究》。这一成果由上海6家单位的数十名研究人员共同合作完成,通过对7000多例临床调查数据,探索非处方紧急避孕药左炔诺孕酮是否增加异位妊娠的发生。上海交大医学院附属国际和平妇幼保健院黄荷凤教授为通讯作者,张健主任、李骋为第一作者。这项最新研究成果强调了对于使用此类避孕方法需要提供明确指导的重要

国际学术刊物《科学报告》在线发表研究论文《左炔诺孕酮紧急避孕药与异位妊娠(宫外孕)风险:一项多中心病例对照研究》。这一成果由上海6家单位的数十名研究人员共同合作完成,通过对7000多例临床调查数据,探索非处方紧急避孕药左炔诺孕酮是否增加异位妊娠的发生。上海交大医学院附属国际和平妇幼保健院黄荷凤教授为通讯作者,张健主任、李骋为第一作者。这项最新研究成果强调了对于使用此类避孕方法需要提供明确指导的重要性以及保证女性充分了解使用紧急避孕药相关的风险。这是全球首次应用多中心大量临床调查数据发表的紧急避孕与女性生殖健康的研究成果。
我国是人口大国,计划生育是国策,避免非意愿妊娠和降低人工流产率更具挑战。1998年始左炔诺孕酮在我国正式作为非处方紧急避孕药应用,其防止非意愿妊娠的效果已得到公认,既往国内外大量临床随机对照研究试验数据表明其安全可靠并不增加异位妊娠发生。由于其有效、便利、安全而迅速受到我国妇女的热衷而得到广泛应用,然而,随着日益广泛应用,其安全性问题(尤其是失败后异位妊娠是否增加?)开始受到关注但始终没有数据证实。
对此,黄荷凤研究团队所在的国际和平妇幼保健院联合上海市第一人民医院、上海市计划生育研究所、松江区中心医院、闵行区中心医院、松江区妇幼保健院等6家医疗机构,共同探讨左炔诺孕酮是否增加异位妊娠风险的问题。
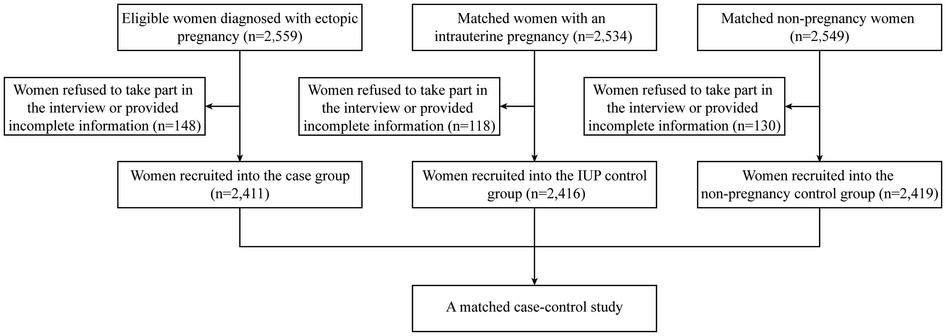
课题组运用流行病学调查研究的方法,对2411例异位妊娠病例、2416例宫内妊娠及2419例非孕妇女进行回顾性病例对照研究,分析表明,服用左炔诺孕酮并不增加异位妊娠风险,然而,一旦避孕失败,异位妊娠风险大于宫内妊娠,尤其见于服药后同一周期再次有无保护性性生活者,以及服药后同一周期再次性生活后重复服用左炔诺孕酮者。研究者在充分肯定左炔诺孕酮紧急避孕药能有效降低非意愿妊娠作用的同时,强调避孕失败后要高度警惕异位妊娠发生风险的增加。因此,黄荷凤表示,“推广合理使用左炔诺孕酮紧急避孕药对保护妇女生殖健康意义重大。”
原始出处:
Zhang J, Li C, Zhao WH, Xi X, Cao SJ, Ping H, Qin GJ, Cheng L, Huang HF.Association between levonorgestrel emergency contraception and the risk of ectopic pregnancy: a multicenter case-control study. Sci Rep. 2015 Feb 12;5:8487. doi: 10.1038/srep08487.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








避孕成功当然各种妊娠(宫内和宫外)风险都降低啊?避孕不成功增加异位妊娠的风险.就是等于药物本身增加异位妊娠风险?我这样理解对吗?
72
额,
149
额,
142
了解,
116
了解,
113
中国学者
80
赞
94
以阅
90
#紧急#
61
#宫外孕#
40