Cardiovasc Diabetol :循环代谢物和分子脂质种类与1型糖尿病未来心血管发病率和死亡率相关
2022-08-01 从医路漫漫 MedSci原创
心血管疾病死亡率过高和寿命缩短主要是由于与普通人群相比,1型糖尿病患者动脉粥样硬化的发病更早,进展更迅速。
背景:尽管对已确立的危险因素进行了更好的控制,但1型糖尿病患者的心血管(CV)发病率和死亡率仍有相当大的风险。因此,需要更好地了解1型糖尿病的潜在病理生理学,以改进风险评估和干预。基于组学的技术可能允许进一步了解1型糖尿病心血管疾病(CVD)的潜在病理生理学,并可能导致识别新的生物标记物和靶点,用于新的治疗或在高危个体中实施现有的治疗。
心血管疾病死亡率过高和寿命缩短主要是由于与普通人群相比,1型糖尿病患者动脉粥样硬化的发病更早,进展更迅速。动脉粥样硬化是由内皮细胞炎症引发的过程,导致巨噬细胞结合,巨噬细胞摄取氧化的低密度脂蛋白并转化为泡沫细胞。泡沫细胞与T细胞和钙化的平滑肌细胞一起形成动脉粥样硬化斑块。由于循环生物分子与血管内皮细胞直接接触,并可能参与动脉粥样硬化的过程,因此利用新型的基于质谱学的组学方法研究代谢途径在心血管疾病领域具有特殊的意义。与传统的生物标志物相比,这些技术可以更全面地描述代谢途径。组学方法虽然还处于早期的技术和科学发展阶段,但已经显示出加深对心血管疾病认识的巨大潜力。此外,我们先前已经提供了关于代谢产物和分子脂质种类如何与1型糖尿病的微血管并发症相关的新见解。
目的:在目前的研究中,我们调查了一大组血清代谢物和分子脂质种类与1型糖尿病患者动脉粥样硬化性心血管疾病发病率和死亡率的关系。
方法:这项研究包括669名1型糖尿病患者。使用质谱仪进行非靶向血清代谢组学和脂类分析。心血管事件(心血管死亡率、冠状动脉疾病、中风和外周动脉干预)的数据来自丹麦健康登记处,并使用COX风险模型进行分析。代谢物和分子脂物种在调整假发现率(FDR)的单变量模型中进行分析。随后在调整后的模型中分析满足pFDR<0.05的代谢物和分子脂质种类,包括年龄、性别、血红蛋白A1c、平均动脉压、吸烟、体重指数、低密度脂蛋白胆固醇、估计的肾小球滤过率、尿白蛋白排泄率和既往心血管疾病。根据甘油三酯和他汀类药物的使用,进一步调整了分子脂类物质的分析。
结果:受试者中男性占55%,平均年龄(55±13)岁。较高的4-羟基苯乙酸(HR 1.35,CI[1.01~1.80],p=0.04)和较低的苏氨酸(HR 0.81,CI[0.67~0.98]p=0.03)与心血管事件的发生有关(n=95)。在脂质组学分析中,二酰基磷脂酰胆碱(PC)(36:2)(HR 0.82,CI[0.70-0.98],p=0.02)、烷基-酰基磷脂酰胆碱(PC-O)(34:2)(HR 0.76,CI[0.59-0.98],p=0.03)和(PC-O)(34:3)(HR 0.75,CI[0.58-0.97],p=0.03)水平较高,与心血管事件的风险较低相关。而较高的鞘磷脂(SM)(34:1)(HR 1.32,CI[1.04-1.68],p=0.02)与风险增加相关。
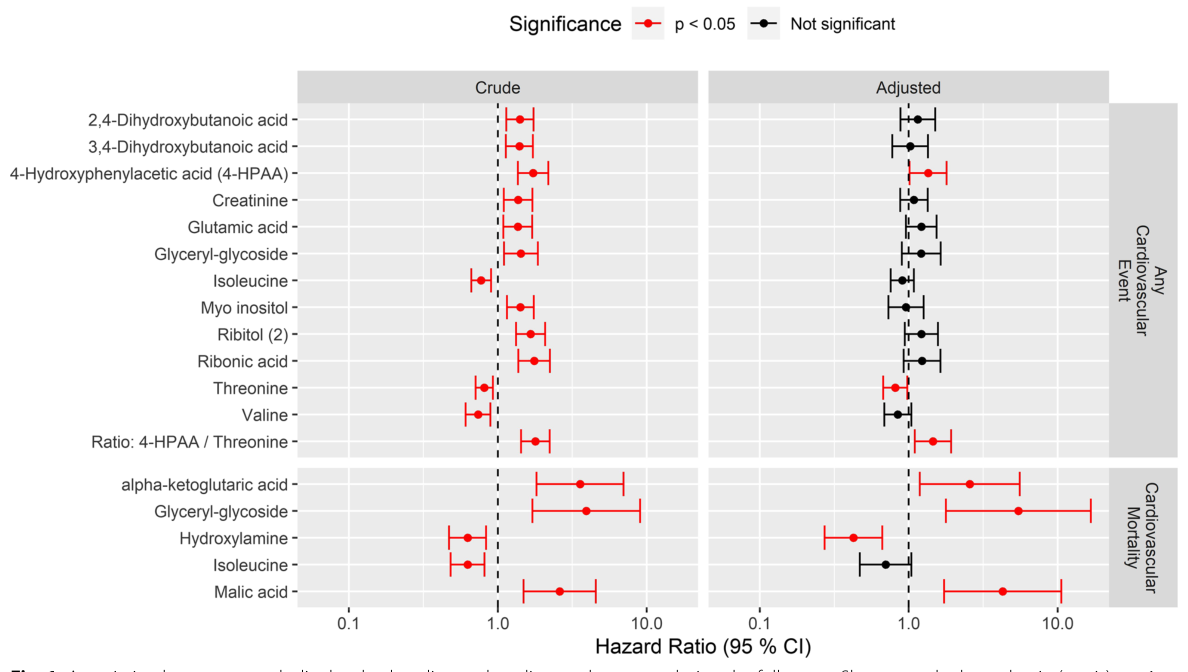
图1基线代谢物水平与随访期间心血管事件之间的关系。显示的是与任何心血管事件(上图)和心血管死亡率(下图)相关的代谢物(行)的风险比(代谢物水平每1SD的x轴)。关联性和95%的可信区间来自原始模型(左图)和根据临床协变量调整后的模型:性别、基线年龄、血红蛋白A1c、平均动脉压、吸烟、体重指数、低密度脂蛋白胆固醇、估计的肾小球滤过率、尿白蛋白排泄率和既往心血管疾病(右图)。图中包括粗关联度小于5%的代谢物,与p<0.05的关联性用红色表示

图2心血管相关分子的基线血液水平(y轴),按是否经历任何心血管事件(n=95)的参与者分层。
个体的血浆代谢物或分子脂质水平用圆点表示,种群分布用小提琴图表示,其中水平线表示四分位数。代谢物显示在第一列,分子类物质显示在另外两列
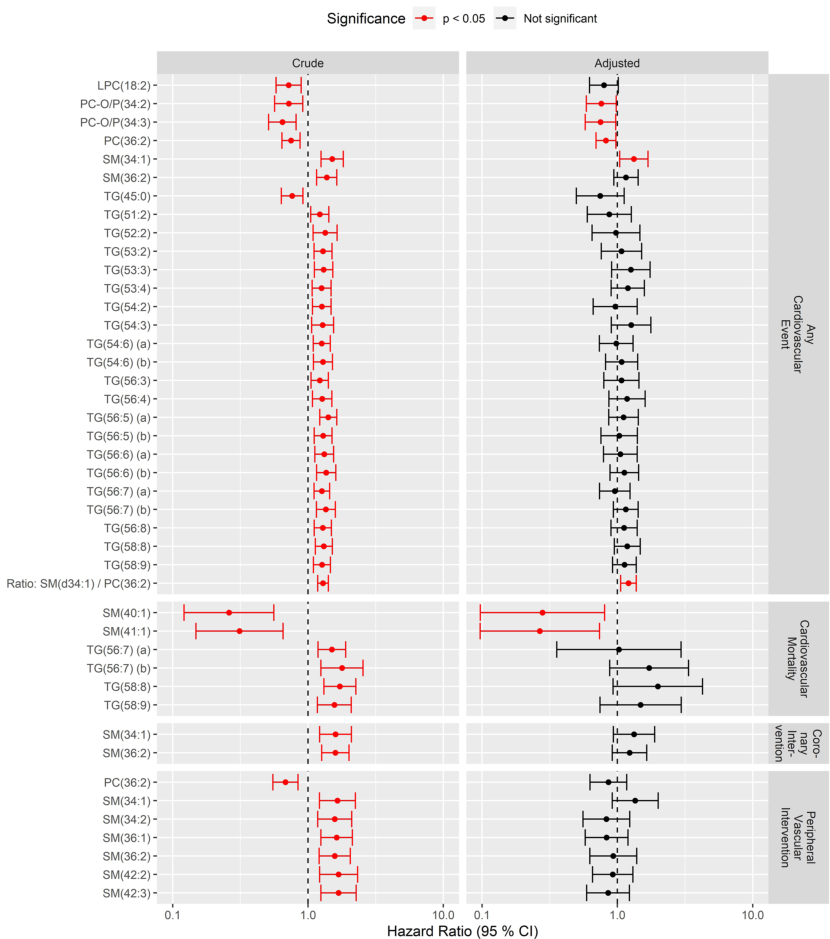
图3基线血脂水平与随访期间心血管事件之间的关系。显示的是与任何心血管事件(上图)和心血管死亡率(下图)相关的分子类物质(ROW)的风险比(x轴)。关联性和95%的可信区间来自原始模型(左图)和根据临床协变量调整后的模型:性别、基线年龄、血红蛋白A1c、平均动脉压、吸烟、体重指数、低密度脂蛋白胆固醇、血浆总甘油三酯、估计的肾小球滤过率、尿白蛋白排泄率、既往心血管疾病和他汀类药物的使用(右图)。图中包括粗缔合度在FDR<5%的分子脂物种,与p<0.05的关联用红色表示
结论:循环代谢产物和分子脂质种类与1型糖尿病患者未来的心血管事件有关。虽然这些生物分子对心血管系统的因果效应尚不清楚,但我们的发现支持,尽管仍处于早期阶段,基于组学的技术可能有可能揭开1型糖尿病心血管疾病领域的新途径和生物标志物的面纱。
原文出处:Ferreira-Divino LF, Suvitaival T, Rotbain Curovic V,et al.Circulating metabolites and molecular lipid species are associated with future cardiovascular morbidity and mortality in type 1 diabetes.Cardiovasc Diabetol 2022 Jul 18;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
57
#ASC#
50
#发病率#
81
#代谢物#
59
#DIA#
38