European Urology:热门靶点CD38在晚期前列腺癌中的作用
2021-06-11 MedSci原创 MedSci原创
CD38可以协同和克服现有的腺苷合成经典靶向治疗的耐药性,并帮助患者选择合理的组合治疗方案。
转移性去势耐药前列腺癌(mCRPC)仍然是一种致命的疾病,总生存期(OS)为2-3年。克服前列腺肿瘤微环境(TME)中的免疫抑制屏障是改善前列腺癌(PC)治疗结果的关键。

Pixabay.com
CD38是核糖环化酶家族的一种胞外酶,表达于免疫祖细胞表面。它的受体、配体和酶功能通过调节免疫调节、代谢、钙介导的信号转导、细胞粘附和迁移等参与肿瘤的发生和进展。CD38催化烟酰胺腺嘌呤二核苷酸的转化最终导致非典型腺苷合成,而单剂腺苷A2A受体阻滞在mCRPC患者中显示出抗肿瘤活性。
简单来说,CD38是一种可药物化的外酶,参与了腺苷的生成,而腺苷与肿瘤免疫逃逸有关,CD38在前列腺肿瘤浸润性免疫细胞(TIICs)中的表达和作用尚未阐明。
近日,有研究者探索了前列腺癌(PC)上皮细胞和TIICs上CD38的表达特征,并将其表达与临床结果联系起来。该研究成果发表在了European Urology期刊上,让我们来一探究竟吧!
研究者对国际癌症/前列腺癌基金会(SU2C/PCF)队列中159例转移性去势抵抗前列腺癌(mCRPC)患者和弗雷德·哈钦森癌症研究中心队列中63例患者的共171例mCRPC样本进行了RNAseq分析。CD38表达通过免疫组织化学评分,并与回顾性收集的临床数据相关联。
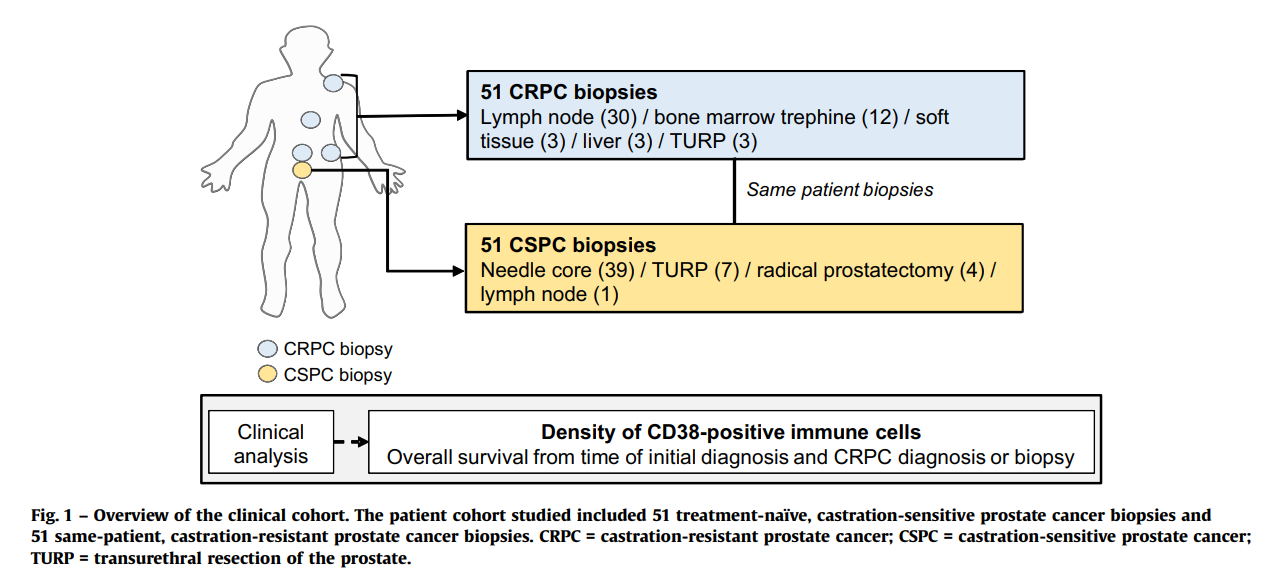
临床队列概述
采用多重免疫荧光法检测PC活检组织中CD38的表达,负二项混合模型分析CSPC和CRPC活检组织中CD38+TIIC密度的差异。采用Cox回归模型进行单变量和多变量生存分析。
分析结果显示,mCRPC中CD38 mRNA的表达与免疫信号通路上调密切相关。CD38 mRNA的表达与白细胞介素IL-12、IL-23和IL-27信号传导以及免疫抑制腺苷和T细胞衰竭信号传导有关。CD38蛋白在B细胞和髓样细胞等表型多样性TIICs中频繁表达,但在肿瘤上皮细胞中大部分不表达。CD38+TIIC密度随CRPC进展而增加,并与较差的总生存率独立相关。未来还需进一步研究TIIC CD38的功能。
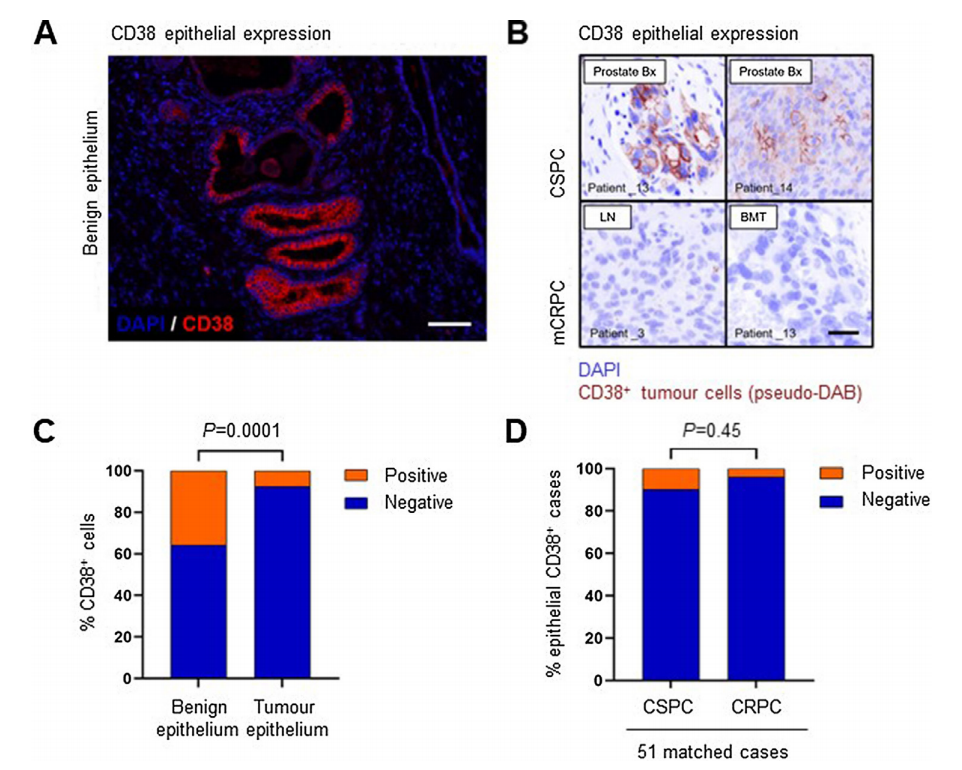
CD38在前列腺癌上皮细胞和良性上皮细胞中的表达
本研究是第一个描述CD38在前列腺上皮细胞和前列腺TIICs上的表达和潜在临床影响的研究,希望评估CD38作为致死性前列腺癌的预后生物标志物,并重新利用CD38定向治疗来消除CD38+TIICs的潜在有害影响。研究人员发现CD38在表型多样的前列腺TIICs上高表达,这些细胞与更差的OS独立相关。
这对探索PC生物标志物和治疗的发展至关重要。CD38可以协同和克服现有的腺苷合成经典靶向治疗的耐药性,其表达可以预测对阻断腺苷合成的现有疗法(如抗CD73和/或抗CD39抗体)的耐药性,并帮助患者选择合理的组合治疗方案。
总之,这些数据支持CD38在TIICs上的表达可以作为一种潜在的预后生物标志物,也证实了未来将CD38作为致死性PC治疗靶点研究的可行性。
参考文献:CD38 in Advanced Prostate Cancers Christina Guo † Mateus Crespo † Bora Gurel Wei Yuan Johann S. de Bono International SU2C PCF Prostate Cancer Dream Team Show all authors Show footnotes Open DOI:https://doi.org/10.1016/j.eururo.2021.01.017
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
90
#热门靶点#
84
#期前列腺癌#
0
#晚期前列腺癌#
85
厉害
83
前列腺癌相关研究,学习了,谢谢梅斯
77