胰腺内分泌肿瘤的分子生物学研究进展
2011-07-29 陈原稼 乔新伟 中国医学论坛报
陈原稼 教授,北京协和医院消化内科研究员,教授,长期从事胃肠激素和肿瘤的研究,曾在美国国立卫生研究院(NIH)从事PET 的分子生物学研究,研究论文曾获欧洲神经内分泌肿瘤学会年会论文一等奖。 对胰腺内分泌肿瘤(Pancreatic Endocrine Tumors,PET)的分子生物学研究不仅有助于了解这类肿瘤发生的分子机制,寻找治疗的分子靶点,还有望发现有助

陈原稼 教授,北京协和医院消化内科研究员,教授,长期从事胃肠激素和肿瘤的研究,曾在美国国立卫生研究院(NIH)从事PET 的分子生物学研究,研究论文曾获欧洲神经内分泌肿瘤学会年会论文一等奖。
对胰腺内分泌肿瘤(Pancreatic Endocrine Tumors,PET)的分子生物学研究不仅有助于了解这类肿瘤发生的分子机制,寻找治疗的分子靶点,还有望发现有助鉴别肿瘤的良恶性病变、判断其预后的分子标志物。
PET是较为罕见的肿瘤,据美国最近发表的流行病学研究结果显示, 从1973年到2004 年,神经内分泌肿瘤(NET)的发病率显著上升, 其中PET的发病率从1973年的略低于0.2例/10万人上升至2004年的0.32例/10万人, 增长超过50%。在欧洲也有相似的报告。
PET是涉及多学科的疑难疾病, 其发生的分子机制不明。由于该类肿瘤临床表现很复杂, 患者往往不能获得及时的诊断。研究显示,多数患者从发病到确诊的时间是4~5年。所以,临床上许多患者确诊时已处于晚期, 失去了最佳的治疗时机。此外,PET良恶性病变的鉴别和患者预后的判断也是临床上的难题。对于多数肿瘤, 病理诊断是鉴别良恶性病变的金标准,PET却不一样,其诊断只能依据临床上是否发现了肿瘤转移和邻近脏器的侵袭, 而非依赖病理专家的形态学判断。所以,部分尚未发生侵袭转移的恶性肿瘤, 即早期的恶性肿瘤不能获得及时的诊断。肿瘤良恶性病变判断正确与否,关系到诊断的准确性和后续的治疗方案, 乃至患者的生命。
因此,对PET的分子生物学研究不仅有助于了解这类肿瘤发生的分子机制,寻找治疗的分子靶点, 还有望发现有助鉴别肿瘤的良恶性病变、判断其预后的分子标志物。
家族遗传性PET发生的分子机制
PET发生的分子机制尚未完全明确, 常见的抑癌基因p53、p16、Rb 和癌基因ras、fos、Src在PET中很少发生改变。
目前家族遗传性PET的发病机制已明确,其中主要是抑癌基因MEN-1 相关的PET,在这部分家族遗传性的肿瘤中,MEN1基因失活导致肿瘤发生。MEN1基因位于染色体11q13,其编码的蛋白质Menin蛋白具有调控细胞的增殖和分化等多种重要的功能。Menin 蛋白可以和转录因子c- jun 结合,从而抑制细胞分裂增生,其还参与甲基转移酶复合体的形成,促使组蛋白H3K4 甲基化,进而激活p27 基因和p18基因的转录, 从而抑制肿瘤的发生。一旦MEN1基因失活[主要是胚系突变和基因杂合缺失(LOH)], 就会导致多发性内分泌腺瘤病1型(MEN-1)的发生, 其中包括 PET。
自从明确MEN1 基因失活导致MEN后,后来的研究发现,约20%的MEN患者和家系未能检测出MEN1基因突变。在这些家系中发现,p27 基因的胚系突变也能导致MEN的发生。此外, 还有极少数家族遗传性PET 的发生与VHL 基因、NF2 抑癌基因失活有关。
散发性PET的分子机制研究进展
在散发性PET 中,部分肿瘤也能发生MEN1基因异常,但绝大部分散发性PET的分子病理机制仍有待进一步的研究。
近年来,国外研究显示,约1/4至1/3的散发性PET发生MEN1基因突变,43%的散发性胃泌素瘤和17%的胰岛素瘤发生了MEN1 基因的LOH。而我们的研究发现,40%的散发性胰岛素瘤发生了MEN1基因的LOH。因此,MEN1基因在少数散发性PET的发生中也发挥一定作用。有研究显示,仅约15%的PET 与VHL基因的异常有关。
今年,《科学》(Science)上发表的一项研究对散发性PET的近18000个编码基因的外显子进行测序。结果发现,44%的肿瘤细胞存在 MEN1基因突变并导致基因失活,未发现K-ras基因和CDKN2A基因的突变,仅有3%的肿瘤有p53基因突变,这与之前的研究结果基本一致。
研究显示,细胞周期蛋白(Cyclin)D1在散发性PET 中高表达,参与肿瘤的发生。而p27基因的失活会导致Cyclin D和CDK4的活性升高。
同样和CDK4 相互作用的P16 蛋白是否参与PET 的发生颇有争议,在PET 不同亚类之间,抑癌基因p16/INK4相关研究的数据不一致。有研究显示,约45%的PET发生了p16/INK4 基因缺失、甲基化及突变,39%的无功能PET和10%的功能性PET发生了p16 /INK4基因LOH;亦有研究表明,散发性PET中未见p16/INK4基因异常。我们针对胰岛素瘤的研究发现,约90%的瘤旁胰岛存在P16蛋白表达,而仅有27%的胰岛素瘤表达该蛋白,约40%的胰岛素瘤发生了p16基因启动子的甲基化。
近年来,不少研究关注PET 的表观遗传学改变,63%~100%的PET存在抑癌基因RASSF1A 启动子区的甲基化。该基因是目前已知的在PET 中甲基化频率最高的基因,尚未明确该基因的失活在PET 发生过程中的作用。
此外,有相当比例的PET 发生O6-MGMT 基因(40%)、错配修复基因hMLH1(23%)和RAR-β 基因的甲基化(25%)。我们最近的研究也发现,约1/3的胰岛素瘤发生hMLH1的甲基化,且该基因启动子的甲基化是导致基因失活的主要机制之一。另外,我们在胰岛素瘤中发现,RAR-β 和MGMT 基因的甲基化率高达90%和86%,显著高于研究报告的40%和25%。这些基因高甲基化的肿瘤生物学意义还有待深入研究。
近日,欧洲学者利用芯片技术检测PET中microRNA 的表达后发现,数十种microRNA在PET中表达上升或下调,其中miR- 221 和miR-222 在PET 中表达上调,这两种microRNA可以和p27/CDKN1B基因的3’端非编码区结合,抑制p27基因的翻译从而降低其蛋白表达水平。因此,miR-221和miR-222 有可能参与PET的发生发展。miR-103、miR-107 和miR-21 的表达在 PET 中也有显著改变,有潜在的肿瘤生物学意义。
PET的分子预后指标
研究认为,PET患者的预后主要取决于肿瘤本身的特性,而与肿瘤分泌激素的多少无关,例如肝转移是胃泌素瘤最为重要的预后指标。
有些临床预后指标往往须较长时间的随访才能获得。此外,Ki-67 免疫组化(IHC)染色阳性率>2%时提示肿瘤有恶性病变的倾向,但Ki- 67的IHC结果并不能反映所有肿瘤的恶性行为。我们研究发现,在胰岛素瘤中,Ki-67 IHC阳性与否和肿瘤的良恶性病变无关。笔者在和欧美学者交流时,有学者也认为,Ki-67作为单一的指标有其局限性。因此,近十年来学者们希望通过探寻分子标志物,以准确地判断PET的预后。
尽管MEN1基因异常对于部分PET的发生至关重要,但该基因异常是否能够预测PET的预后尚有争议。既往研究普遍认为,MEN1基因突变或 LOH与PET患者预后无关,但近期有研究发现,与MEN1基因野生型PET 患者相比,突变型患者生存期显著延长(P=0.01)。该研究提示,MEN1基因突变是PET患者预后良好的分子标志物。
在今年欧洲神经内分泌肿瘤学会年会上,有部分专家认为,应重新认识和评估MEN1基因在PET中的预后价值。
美国NIH 的研究显示,胃泌素瘤中表皮生长因子受体(EGFR)和肝细胞生长因子受体(HGFR)的过表达与胃泌素瘤肝转移及肿瘤治愈率下降显著相关(P值分别为 0.034和0.027)。研究还发现,在胃泌素瘤中,癌基因HER2/neu(EGFR 家族成员)信使RNA(mRNA)的过表达也与胃泌素瘤肝转移显著相关,这提示EGFR、HGFR 和HER2/neu的过表达在胃泌素瘤中有一定的预后价值。另外,1号染色体长臂的LOH 与胃泌素瘤患者的预后差显著相关。
我们的研究首次发现,1 号和22 号染色体长臂的LOH和胰岛素瘤的恶性相关:发生染色体1q21.3-23.2 LOH 的胰岛素瘤有 58%为恶性,而该区域无LOH的肿瘤仅8% 为恶性(P=0.014);此外,发生染色体22q13.3 LOH的胰岛素瘤有43%为恶性,而无该 LOH的肿瘤仅8%为恶性(P=0.009)。而之后荷兰学者发表的研究亦发现,染色体1q23.2和22q13的LOH与胰岛素瘤的恶性相关。
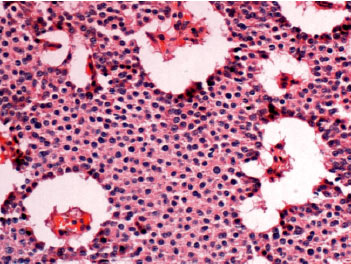
图1 胰岛素瘤的HE染色
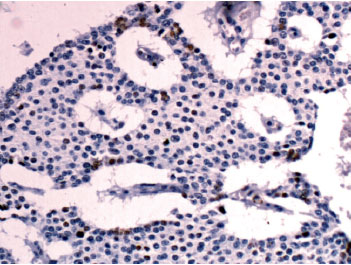
图2 IHC 示肿瘤细胞核中MHL-1 蛋白表达丢失
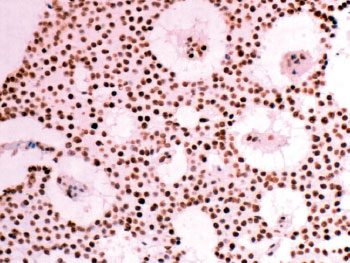
图3 IHC 示hMSH2 蛋白的表达
2009年,我们研究发现,散发性胰岛素瘤存在广泛的微卫星不稳定和错配修复基因MHL-1 表达的下降(见上图)。微卫星不稳定和MHL-1 蛋白表达下降与胰岛素瘤的恶性显著相关(P=4.8×10-6 和P=0.033),且与患者预后差显著相关(P=0.001 和P=0.006)。此外,研究还发现,33%的恶性胰岛素瘤存在hMSH2蛋白表达下调,而在良性肿瘤中这种下调发生率仅为5%(P=0.019)。这提示,DNA错配修复基因异常可能是胰岛素瘤发生和进展的机制之一,且检测基因表达下降和微卫星不稳定可作为鉴别散发性胰岛素瘤良恶性病变的分子标志物。
近日,我们和美国纪念斯隆-凯特林(Memorial Sloan-Kettering)癌症中心及加州大学洛杉矶分校(UCLA)希达西奈山(Cedars-Sinai)医学中心合作,首次在随访的约200 例PET 患者中发现: 肿瘤表达NF-66蛋白患者的总生存率显著高于不表达NF- 66蛋白者(P=0.02),该蛋白的表达和肿瘤良恶性显著相关(P=0.001)(研究尚未正式发表)。这提示,NF-66 蛋白可作为PET患者预后和良恶性病变鉴别的分子标志物。
展望
尽管PET是较为罕见的肿瘤,但近年来对这类肿瘤的研究却并不少见。PET分子生物学研究取得的进展会极大地提高该类肿瘤的诊断、预后判断和治疗水平。例如,《新英格兰医学杂志》在今年2月发表的研究证实,使用雷帕霉素(mTOR)抑制剂治疗分化好的晚期胃肠胰腺神经内分泌肿瘤已获得较为理想的效果。这些治疗原理正是基于肿瘤mTOR信号通路的分子生物学研究而发展的。
总体来说,目前散发性PET 的发病机制仍不明确,因为PET包括多种亚类,例如胃泌素瘤、胰高血糖素瘤、胰岛素瘤和无功能胰腺内分泌瘤等,这些肿瘤既有共同点也有异质性,其发病的分子机制或许有所差异。因此,PET的分子病理机制比我们预期想象的要复杂很多,而肿瘤的分子标志物有着非常重要的临床实用价值,值得进一步探索。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#分子生物学#
56
#肿瘤的分子生物学#
52
#内分泌肿瘤#
52
#分泌#
53
#研究进展#
0
#生物学#
44