Cell:GPR17受体可能成为肥胖的新靶点
2012-06-17 T.Shen 生物谷
近日,来自哥伦比亚大学医学中心(UCMC)的研究者发现了一种大脑受体在调节机体饮食上扮演着中枢的作用。这项研究发现刊登在了近日的国际杂志Cell上。研究者Domenico表示,我们发现的这个受体可以调节进食量。这个受体或可成为新药的一个靶点。 在这项研究中,关于治疗肥胖的新靶点上,研究者重点关注下丘脑,下丘脑可以调节人的食欲。大量的研究已经表明这种调节机制依赖于一种称为AgRP的神经肽,但是具体

近日,来自哥伦比亚大学医学中心(UCMC)的研究者发现了一种大脑受体在调节机体饮食上扮演着中枢的作用。这项研究发现刊登在了近日的国际杂志Cell上。研究者Domenico表示,我们发现的这个受体可以调节进食量。这个受体或可成为新药的一个靶点。
在这项研究中,关于治疗肥胖的新靶点上,研究者重点关注下丘脑,下丘脑可以调节人的食欲。大量的研究已经表明这种调节机制依赖于一种称为AgRP的神经肽,但是具体什么因子影响AgRP的表达,目前尚不清楚。
研究者通过追寻胰岛素和瘦素在机体中的作用发现了一些线索,这两种激素不仅涉及维持机体的能量平衡,而且可以影响AgRP。关闭胰岛素或者瘦素途径会影响食欲,因此研究者假设这两种途径如果同时被关闭将会影响摄食行为。
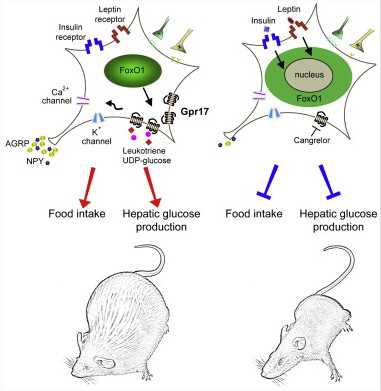
为了验证这种假设,研究者构建了缺失胰岛素和瘦素信号途径的小鼠,正如研究者所假设,去除蛋白质Fox01对于动物摄食有很大的影响,缺少Fox01的小鼠相比正常小鼠吃的较少,脂肪较少,而且其在葡萄糖平衡和瘦素、胰岛素敏感性上有很好的平衡性。Fox01并不是一个很好的新药靶点,因此研究者试图去寻在别的方法,使用基因表达谱的方法,研究者发现了一个基因在正常AgRP神经元细胞的小鼠中高度表达,而且可以在Fox01缺失的小鼠中沉默。这个基因命名为Gpr17(G蛋白偶联受体17),可以产生细胞表面受体Gpr17。
为了证明该受体确实可以介导食欲控制,研究者将Gpr17激活剂注入正常小鼠中,结果小鼠的食欲增加。相反的,当给与Gpr17抑制剂,小鼠的食欲会下降。注射入Fox01缺失的小鼠中并没有产生明显效应。
研究者Accili表示,在人类机体中也发现了Gpr17受体,这将作为治疗肥胖疗法的一个新靶点,Gpr17是G蛋白偶联受体受体家族的成员之一,而且其高度受药物控制。研究者的研究标题为“G蛋白偶联受体GPR17可以介导AgRP神经元细胞FoxO1最终引发食欲效应”相关研究由美国国立卫生院提供支持。

doi:10.1016/j.cell.2012.04.032
PMC:
PMID:
FoxO1 Target Gpr17 Activates AgRP Neurons to Regulate Food Intake
Hongxia Ren, Ian J. Orozco, Ya Su, Shigetomo Suyama, Roger Gutiérrez-Juárez, Tamas L. Horvath, Sharon L. Wardlaw, Leona Plum, Ottavio Arancio, Domenico Accili
Hypothalamic neurons expressing Agouti-related peptide (AgRP) are critical for initiating food intake, but druggable biochemical pathways that control this response remain elusive. Thus, genetic ablation of insulin or leptin signaling in AgRP neurons is predicted to reduce satiety but fails to do so. FoxO1 is a shared mediator of both pathways, and its inhibition is required to induce satiety. Accordingly, FoxO1 ablation in AgRP neurons of mice results in reduced food intake, leanness, improved glucose homeostasis, and increased sensitivity to insulin and leptin. Expression profiling of flow-sorted FoxO1-deficient AgRP neurons identifies G-protein-coupled receptor Gpr17 as a FoxO1 target whose expression is regulated by nutritional status. Intracerebroventricular injection of Gpr17 agonists induces food intake, whereas Gpr17 antagonist cangrelor curtails it. These effects are absent in Agrp-Foxo1 knockouts, suggesting that pharmacological modulation of this pathway has therapeutic potential to treat obesity.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Cell#
68
#CEL#
50
#新靶点#
0