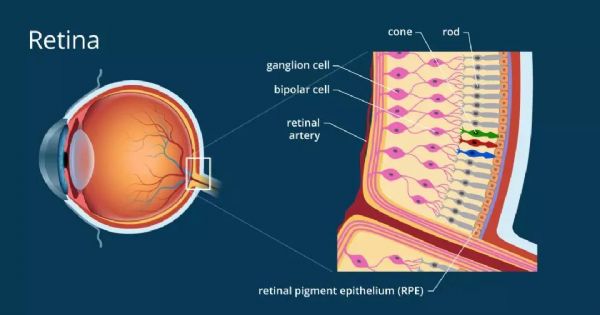
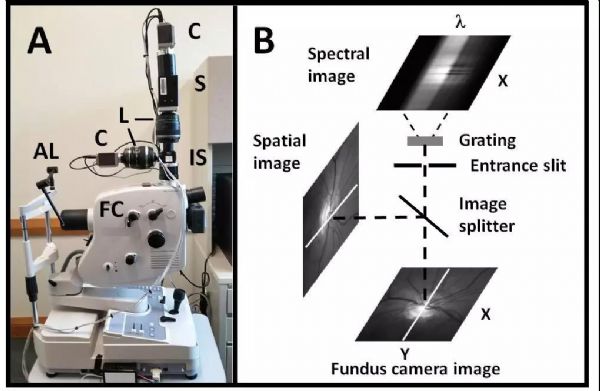
ACS Chem Neurosci:如何从视网膜看出阿尔兹海默病端倪?
2019-11-15 Blake 转化医学网
阿尔茨海默病是一种常见的神经退行性疾病,也是导致痴呆的主要原因。阿尔茨海默病患者认知能力会下降,然而其分子病理则开始于出现临床症状前数十年,因此迫切需要发现在阿尔茨海默病早期具有高敏感度的生物标志物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#视网膜#
82
#ACS#
81
#ROS#
68
#阿尔兹海默#
72
非常精彩,受益非浅
101