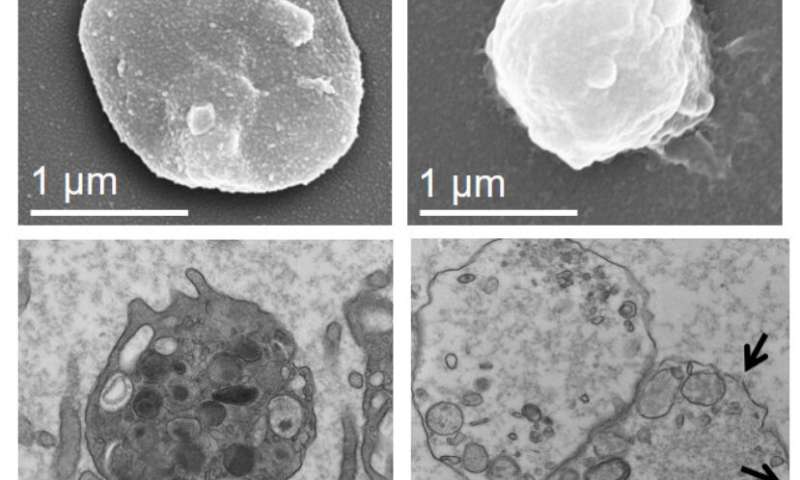
NEJM:血栓性血小板减少性紫癜-病例报道
2019-04-18 xing.T 网络
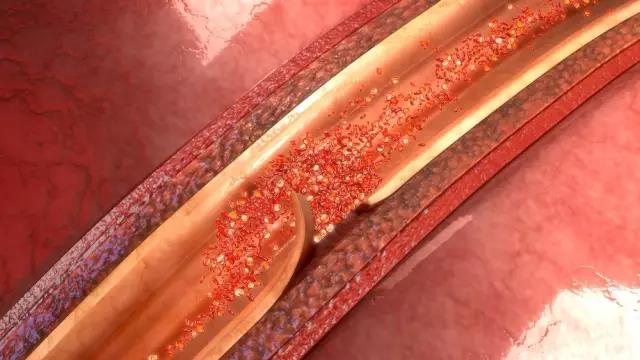
该患者立即开始血浆交换以治疗疑似血栓性血小板减少性紫癜。如果没有及时开始治疗,血栓性血小板减少性紫癜的死亡率很高。患者接受血浆置换并接受静脉注射甲基强的松龙5天,症状消失,血小板计数增加。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



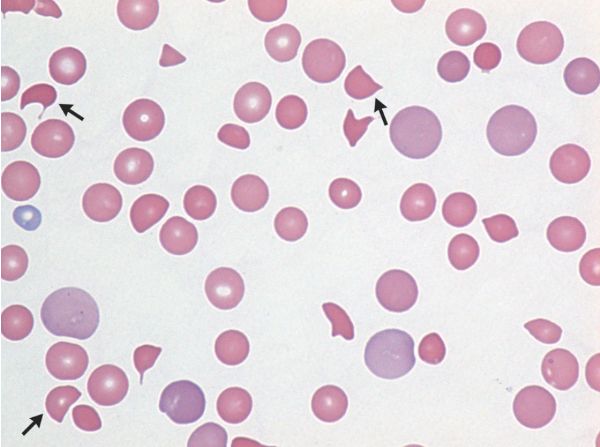






#血小板减少性紫癜#
0
#血栓性#
59
#血小板减少#
0
#紫癜#
96
#血栓性血小板减少性紫癜#
80
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
118