Diabetes Care:人体中,是否存在肠促胰素—心房钠尿肽轴呢?
2015-01-06 angletears 译 MedSci原创
心房钠尿肽(atrial natriuretic peptide, ANP)是由心房肌细胞合成并释放的肽类激素,人血液循环中的ANP由28个氨基酸残基组成。ANP的主要作用是使血管平滑肌舒张和促进肾脏排钠、排水。当心房壁受牵拉时(如血量过多、头低足高位、中心静脉压升高和身体浸入水中)均可刺激心房肌细胞释放ANP。 2013年,Kim M和他的团队证明,在小鼠实验中,GLP-1受体激动剂通过刺
心房钠尿肽(atrial natriuretic peptide, ANP)是由心房肌细胞合成并释放的肽类激素,人血液循环中的ANP由28个氨基酸残基组成。ANP的主要作用是使血管平滑肌舒张和促进肾脏排钠、排水。当心房壁受牵拉时(如血量过多、头低足高位、中心静脉压升高和身体浸入水中)均可刺激心房肌细胞释放ANP。
2013年,Kim M和他的团队证明,在小鼠实验中,GLP-1受体激动剂通过刺激心房钠尿肽的释放,产生抗高血压的作用。那么,GLP-1是否可以直接影响人体的利尿钠肽系统呢?
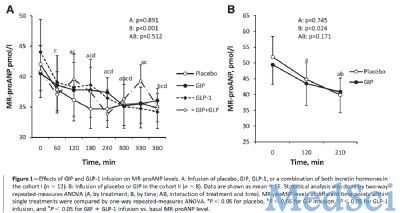
进来,德国的Natalia Rudovich带着这个问题,进行了一项研究,以探讨两种主要的肠促胰岛素,外源性的GIP和GLP-1,对2型糖尿病患者的ANP是否有影响。在2型糖尿病组,选取9名男性和3名女性作为受试者,平均年龄为61±10岁,BMI为30.0±3.7 kg/m2,HbA1c 7.3±1.5%。试验方法:在不同日随机给予以下处理:安慰剂(1%的人血白蛋白液加入0.9%的氯化钠),GIP(4 pmol•kg ˉ1•minˉ1),GLP-1(7–36)-amide(4 pmol•kg ˉ1•minˉ1),或者两种肠促胰素联合治疗360min分钟以上。另外,选取8名超重但糖耐量正常的男性个体(49.9±3.2 岁,BMI 32.9±0.7 kg/m2),给予GIP(2 pmol•kg ˉ1•minˉ1)和安慰剂(等渗盐水)静注240min。
在2型糖尿病患者中,外源性GIP可以使体内总的GIP稳定在530 pmol/L水平,而完整的有生物活性的GIP稳定在225 pmol/L水平;静注GLP-1,血浆中总的GLP-1稳定在145pmol/L水平,而完整的有生物活性的GLP-1稳20pmol/L。
而在GIP治疗组,在静注GIP的最后1小时,proANP水平有轻微的下降。在试验组之间,没有发现proANP的浓度的存在明显不同。
在健康的超重个体中,静注外源性GIP期间,总的GIP水平稳定在120 pmol/L,而安慰剂(生理盐水组)组是5 pmol/L。proANP水平在GIP静注组和安慰剂组都下降了,但是没有发现两组之间proANP的水平有差别。
Natalia Rudovich等人结果发现,在2型糖尿病个体中,药理学水平上的GIP和/或GLP-1均不能刺激ANP的分泌。
此外,有试验观察到ProANP的水平在进餐时是下降的,这就说明调节proANP的是饮食相关的因素,而不是肠促胰岛素或者ANP的水平本身就有白昼周期变化。文章指出这篇研究的局限是在于样本量小,样本接受肠促胰岛素处理的时间短。总之,本研究不能证明人体也存在肠促胰素—ANP轴。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#BET#
70
#DIA#
73
#Diabetes#
0
#肠促胰素#
78
#钠尿肽#
90
#心房钠尿肽#
65
#心房#
58