NEJM:室性心动过速患者使用导管消融优于抗心律失常药物
2016-05-06 MedSci MedSci原创
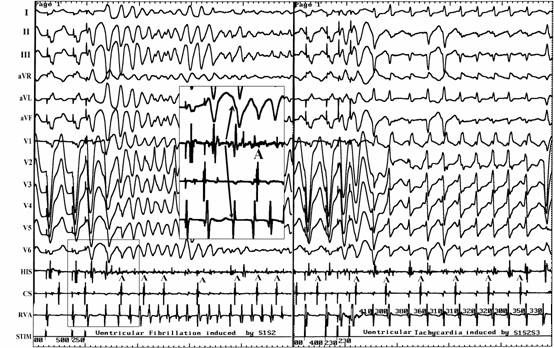
带有植入式心律转复除颤器(ICD)心肌梗死的幸存者尽管服用抗心律失常药物治疗,但发生复发性室性心动过速也非常频繁。解决这个问题最有效的管理方法是不确定的。原始出处:John L. Sapp,George A. Wells,Ratika Parkash,et al.Ventricular Tachycardia Ablation versus Escalation of Antiarrhythmic
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习啦,不错
115
#导管消融#
73
#室性心动过速#
83
#消融#
79
#心动过速#
70
#抗心律失常药物#
96