Heart:运动习惯改变与心血管事件后死亡率的关系
2022-05-22 MedSci原创 MedSci原创
在患有心血管疾病的老年人中,更良性的运动习惯变化轨迹与更低的死亡率相关。该研究的结果支持心血管疾病的老年人进行体育活动。
此前的研究已经证明,养成锻炼习惯与死亡风险呈负相关。目前的指南建议定期锻炼以降低全因或心血管疾病死亡和发病率的风险。然而,支持锻炼对心血管疾病(CVDs)老年人益处的证据很少,因为锻炼和死亡率的研究主要是在健康和中年人中完成的。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究旨在探究老年人心血管事件后运动习惯改变与死亡率之间的关系。

研究人员分析了2003-2012年期间60岁以上、在诊断心血管疾病(CVD)前后2年内连续两次体检的老年人运动习惯改变与全因、心血管疾病和非心血管疾病死亡之间的关系。根据锻炼习惯的变化,他们被分为四组:一直不锻炼的人、放弃锻炼的人、新近锻炼的人和持续锻炼的人。基线特征的差异使用治疗加权的逆概率进行了调整。
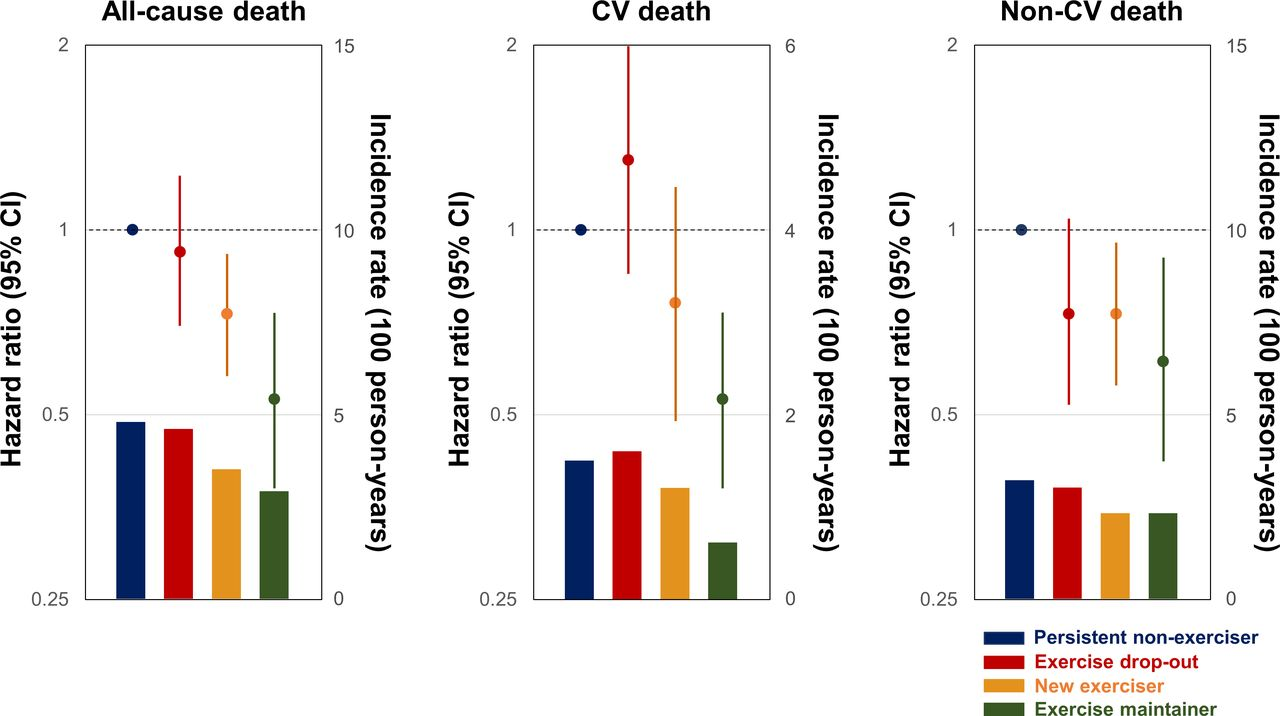
6076例患者中位年龄为72岁(IQR为69-76),男性占50.6%。与持续不运动者(发病率(IR)为4.8/100人年)相比,新近运动者(IR为3.5,HR为0.73,95%CI为0.58~0.91)和持续运动者(IR为2.9,HR为0.53,95%CI为0.38~0.73)与全因死亡风险降低相关。新近运动者(IR为2.3,HR为0.73,95%CI为0.56-0.95)和持续运动者(IR为2.3,HR为0.61,95%CI为0.42-0.90)的非心血管疾病死亡率显著低于一直不运动者(IR为3.2)。此外,研究人员观察到了新近锻炼者和持续锻炼者的心血管死亡风险有降低的趋势(趋势p值<0.001)。
由此可见,在患有心血管疾病的老年人中,更良性的运动习惯变化轨迹与更低的死亡率相关。该研究的结果支持心血管疾病的老年人进行体育活动。
原始出处:
Dong-Seon Kang.et al.Association between exercise habit changes and mortality following a cardiovascular event.heart.2022.https://heart.bmj.com/content/early/2022/05/18/heartjnl-2022-320882
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管事件#
95
认真学习~~
70
#ART#
56
#HEART#
56