NEJM:三尖瓣关闭不全- Lancisi’s 征案例报道
2016-01-16 MedSci MedSci原创
男性,60岁,既往患有非缺血性心肌病,因最近2-3个星期出现渐进性呼吸困难及体重明显增加9Kg入院就诊。体格检查中,发现该男子在吸气时胸骨左缘出现明显的收缩期杂音,并随吸气的加深而增强。颈部检查可见明显的颈静脉搏动,称为Lancisi’s 征(请点击原始链接观看视频)。经胸行超声心动图检查显示三尖瓣环形扩张,导致严重的关闭不全。Lancisi’s 征是三尖瓣严重返流的临床表现。一般情况下,三峰两谷
男性,60岁,既往患有非缺血性心肌病,因最近2-3个星期出现渐进性呼吸困难及体重明显增加9Kg入院就诊。
体格检查中,发现该男子在吸气时胸骨左缘出现明显的收缩期杂音,并随吸气的加深而增强。
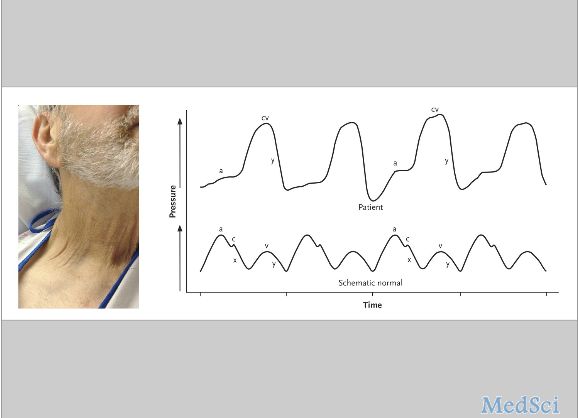
颈部检查可见明显的颈静脉搏动,称为Lancisi’s 征(请点击原始链接观看视频)。
经胸行超声心动图检查显示三尖瓣环形扩张,导致严重的关闭不全。
Lancisi’s 征是三尖瓣严重返流的临床表现。
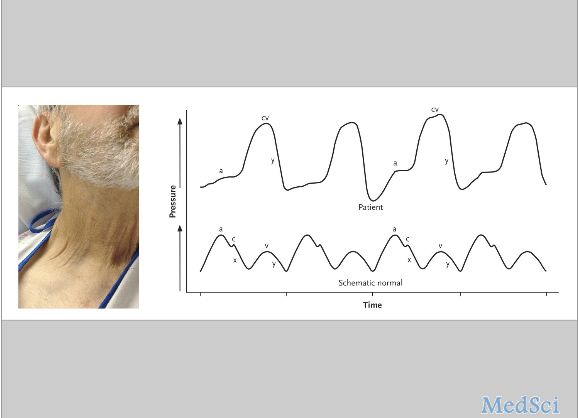
一般情况下,三峰两谷描述的是静脉波形(图中下边的波形是比较具有代表性的正常波形表现)。第一高峰,是舒张晚期心房收缩时所产生的波形。其次,在早期心室等容收缩引起的三尖瓣关闭,产生C波。第三个波峰(V波),发生在收缩晚期心房充盈时。最后,在舒张早期由于学业回流导致心室被动充盈从而产生Y波形下降。在三尖瓣关闭不全的情况下,逆行血流进入右心房心室收缩导致X下降,形成一个融合的CV波。在体表形成我们看到的颈内静脉搏动。此波动通常是由右心房和右心室之间的压力梯度变化的增强所导致的。
André M. Mansoor, M.D., and Steven E. Mansoor, M.D., Ph.D. N Engl J Med 2016; 374:e2January 14, 2016DOI: 10.1056/NEJMicm1502066
http://www.nejm.org/doi/full/10.1056/NEJMicm1502066本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CIS#
86
#NCI#
80
这篇文章有一定深度
147
是一篇不错的文章
156
值得进一步关注
141
不错,赞一个
142
#三尖瓣#
56