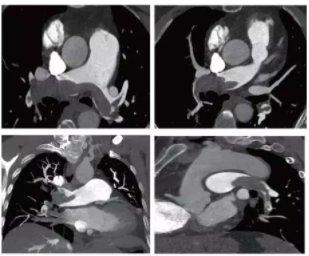
病例分享:急诊来了位大面积肺栓塞病人,惊动了6个学科的主任
2017-12-09 安贞团队 中国医学论坛报今日循环
肺栓塞发病凶险,多数病人都未能得到及时诊断和有效救治。今天我们要介绍的这位病人,不幸中的万幸是,她获得了安贞医院多学科专家团队的携手救治,最终化险为夷。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#大面积肺栓塞#
42
#大面积#
0
谢谢!分享谢谢
63
学习学习谢谢!
74
学习了.谢谢作者分享!
71
肺栓塞发病凶险.多数病人都未能得到及时诊断和有效救治.今天我们要介绍的这位病人.不幸中的万幸是.她获得了安贞医院多学科专家团队的携手救治.最终化险为夷.
67
学习
68
努力学习学习学习
39
学习了感谢分享
41