Stroke:活动性颅内动脉粥样硬化病的诊断和管理
2018-07-29 杨中华 脑血管病及重症文献导读
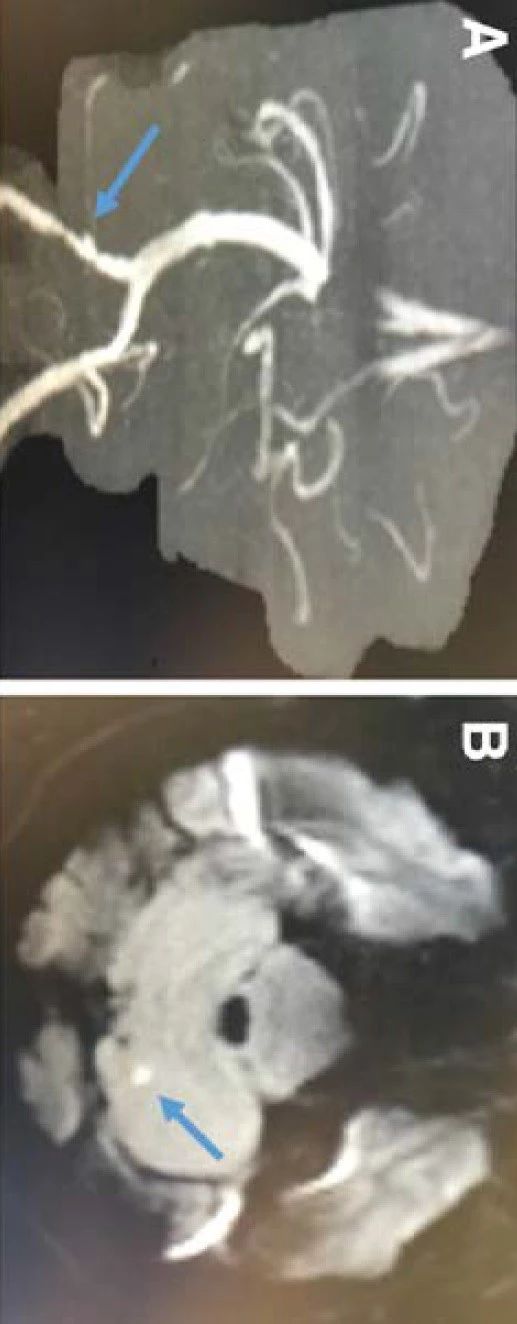
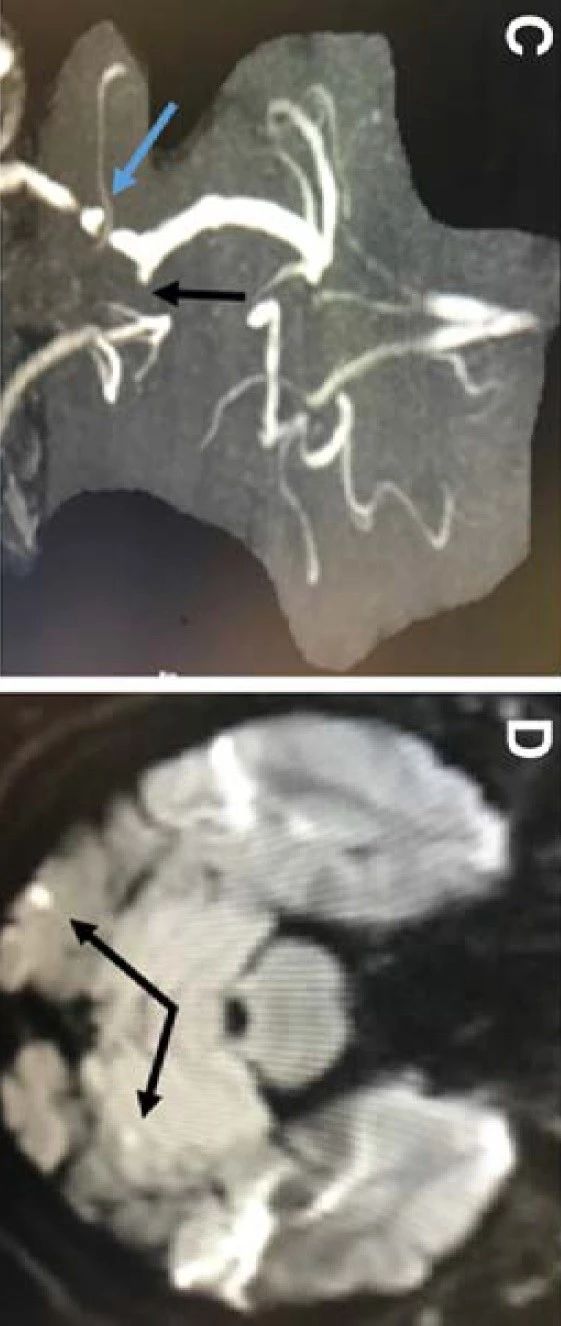
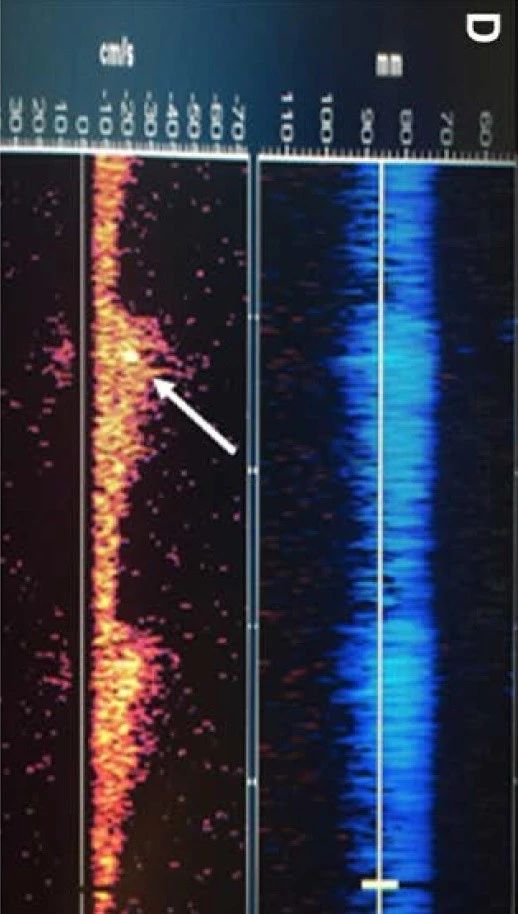
颅内动脉粥样硬化性疾病(ICAD)是缺血性卒中的主要病因,常见于亚洲人、黑人和西班牙种群。MCA最常受累,其次是基底动脉、颈内动脉和椎动脉。ICAD的危险因素包括年龄、高血压、高脂血症和糖尿病。ICAD的卒中机制包括远端灌注受损,斑块破裂导致远端栓塞或分支闭塞。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#活动性#
86
#粥样硬化#
65
#诊断和管理#
77
#颅内动脉粥样硬化#
76
活动性颅内动脉粥样硬化,学习了。
94
阅
107