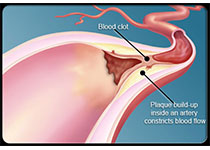
Eur Radiol:颈动脉出血性斑块那可是易损斑块,得好好检查检查!
2017-12-13 shaosai MedSci原创
本研究旨在探究即时非强化血管造影和斑块内出血(SNAP)成像在显示斑块内出血(IPH)的特点,并将其与磁化率准备快速采集梯度回波(MP-RAGE)序列进行比较,研究人员将研究结果发表在Eur Radiol上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#颈动脉#
72
学习了.谢谢分享!
126
6
104
#斑块#
58
好
96