Eur J Nucl Med Mol Imaging:采用PERCIST预测食管鳞癌患者对新辅助化疗的肿瘤反应和预后
2021-05-06 MedSci原创 MedSci原创
部分代谢反应根据SULpeak反应(-50%)进一步分类而改良的PERCIST可能比PERCIST1.0更适合用于评估肿瘤反应,并对复发和预后不良的高危患者进行分层
食道癌是全球第八大常见癌症。经食管切除术治疗的食道癌的5年生存率约为54.5%。伴病理性淋巴结转移(LNM)的食管癌的复发率显着较高,为40%–70%。
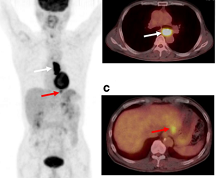
本研究旨在探讨实体肿瘤正电子发射断层显像反应标准1.0(PERCIST1.0)在预测肿瘤对新辅助化疗的疗效和预后方面的价值,并确定是否有必要对食管鳞癌(ESCC)患者进行PERCIST改进。
研究人员分析了177例ESCC患者,评估了PERCIST与其病理反应之间的相关性。采用Kaplan-Meier分析和Cox比例风险模型评估了Whole-PERCIST与无进展生存期(PFS)和总生存期(OS)的关系。此外,为了调查PERCIST的潜在改进方法,研究人员还使用生存树技术分析了患者的预后。
原发性肿瘤的病理反应与PERCIST显著相关(p<0.001)。原发肿瘤SULpeak反应对病理反应的最佳分界值为-50.0%。SULpeak反应的诊断准确率为87.3%,敏感度为54.1%,特异性为68.9%,阳性预测值为60.5%,阴性预测值为84.1%。
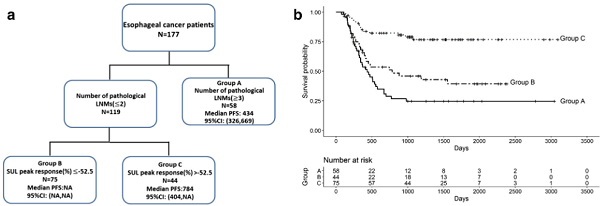
据生存树分析的不同亚组的PFS
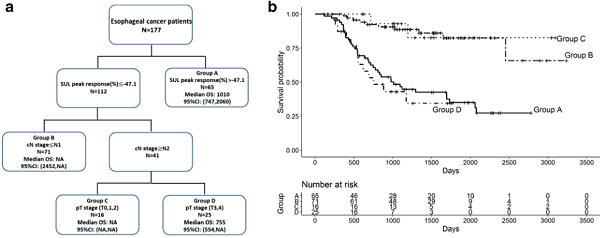
此外,Whole-PERCIST还与PFS和OS显著相关。生存树分析结果显示,SULpeak反应的高度降低与患者的预后显著相关。预测PFS预后和OS预后的临界值分别为-52.5和-47.1%。
根据生存树分析的不同亚组的OS
总而言之,PERCIST1.0有助于预测肿瘤对治疗的反应和预后。然而,在组织病理学反应评估中,18F-FDG-PET/CT往往可能会低估残留肿瘤病灶。部分代谢反应根据SULpeak反应(-50%)进一步分类而改良的PERCIST可能比PERCIST1.0更适合用于评估肿瘤反应,并对复发和预后不良的高危患者进行分层。
原始出处:
Kaida, H., Kitajima, K., Nakajo, M. et al. Predicting tumor response and prognosis to neoadjuvant chemotherapy in esophageal squamous cell carcinoma patients using PERCIST: a multicenter study in Japan. Eur J Nucl Med Mol Imaging (2021). https://doi.org/10.1007/s00259-021-05365-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
73
#鳞癌患者#
96
#新辅助#
118
#CIS#
68
#食管#
80
#鳞癌#
91
#Med#
74
学习
110