ACCF/AHA/HRS发布2012版心律失常器械治疗指南
2012-10-03 赵洁慧 译 中国医学论坛报
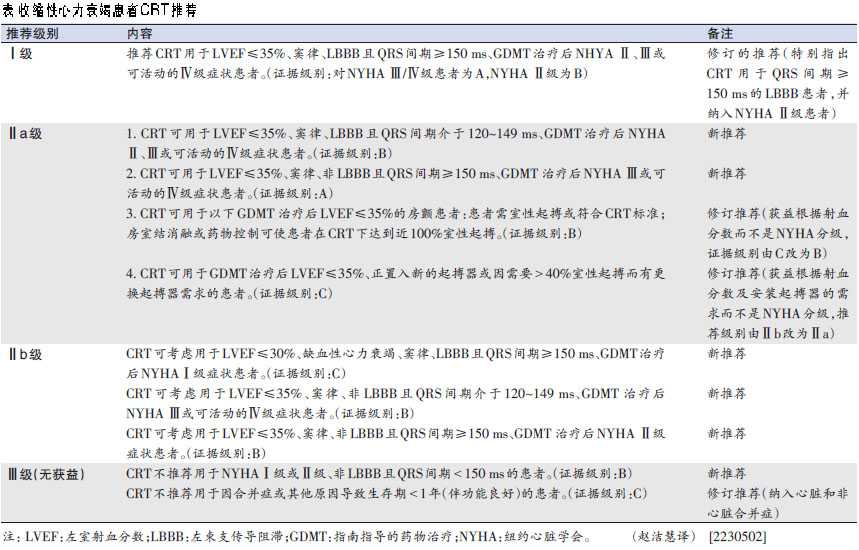
美国心脏病学会基金会(ACCF)、美国心脏学会(AHA)和美国心律协会(HRS)近日联合发布了《2012版心律失常器械治疗指南》,对收缩性心力衰竭患者的心脏再同步化治疗(CRT)作了较多更新(表)。9月10日,新版指南同时在线发表于《美国心脏病学会杂志》(J Am Coll Cardiol)、《循环》(Circulation)、《美国心胸外科杂志》(J
美国心脏病学会基金会(ACCF)、美国心脏学会(AHA)和美国心律协会(HRS)近日联合发布了《2012版心律失常器械治疗指南》,对收缩性心力衰竭患者的心脏再同步化治疗(CRT)作了较多更新(表)。9月10日,新版指南同时在线发表于《美国心脏病学会杂志》(J Am Coll Cardiol)、《循环》(Circulation)、《美国心胸外科杂志》(J Thorac Cardiov Sur )和《心律学》(Heart Rhythm)杂志。
注: LVEF:左室射血分数;LBBB:左束支传导阻滞;GDMT:指南指导的药物治疗;NYHA:纽约心脏学会。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









如果能配上指南原文连接就更好了
186
#治疗指南#
65
#AHA#
60
#ACC#
62
#HRS#
64
#ACCF#
114