CastellviⅡa型腰椎骶化并L4~5及L5~S1椎间盘突出1例
2018-10-20 侯黎升 白雪东 葛丰 临床骨科杂志
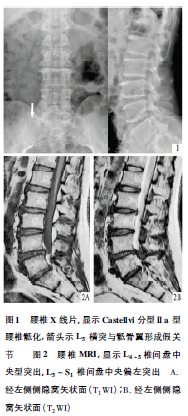
患者,男,60岁。左下肢放射痛5年,加重伴腰痛1年,于2016年9月26日入院。曾于2016年4月在外院行腰椎MRI检查,显示L4~5、L5~S1椎间盘突出,正规非手术治疗5个月无效。查体:L4~5、L5~S1棘突间压叩痛,左下肢直腿抬高试验40°(+),左小腿外侧感觉减退,左胫前肌肌力4+级,拇背伸肌力4级。L5及S1神经根呈受损表现。X线片显示L5右侧横突肥大,同骶骨翼形成假关节,为Caste
临床资料
患者,男,60岁。左下肢放射痛5年,加重伴腰痛1年,于2016年9月26日入院。曾于2016年4月在外院行腰椎MRI检查,显示L4~5、L5~S1椎间盘突出,正规非手术治疗5个月无效。查体:L4~5、L5~S1棘突间压叩痛,左下肢直腿抬高试验40°(+),左小腿外侧感觉减退,左胫前肌肌力4+级,拇背伸肌力4级。L5及S1神经根呈受损表现。X线片显示L5右侧横突肥大,同骶骨翼形成假关节,为CastellviⅡa型腰骶移行椎,属腰椎骶化,见图1。CT显示L4~5椎间盘中央型突出,双侧L5神经根湮没;L5~S1椎间盘中央偏左型突出,左侧S1神经根受压;右侧L5横突与骶骨翼形成假关节。CT矢状面重建证实了轴位CT所见,同时发现L2~3椎间盘右旁侧突出。腰椎MRI扫描显示L4~5椎间盘中央型突出,L5~S1椎间盘中央偏左突出,同CT所见,见图2。
讨论
行选择性神经根封闭,每处注入2%利多卡因1ml,先封闭左S1神经根,放射痛缓解30%,再封闭左L5神经根,放射痛完全消失。确定L4~5及L5~S1椎间盘均为责任节段。L2~3为无症状性椎间盘突出。封闭后2~4h疼痛重现。于9月28日在全身麻醉下手术,术中见L4~5双侧黄韧带肥厚,L4~5椎间盘突出,双侧L5神经根受压,左侧侧隐窝狭窄,行L4~5黄韧带切除,椎间盘摘除,左侧隐窝扩大;L5~S1椎间盘左旁侧突出,S1神经根受压,行椎间盘摘除。然后L4~5椎间左右各植入1枚cage,L5~S1椎间自左后向右前植入1枚cage,L4~S1椎弓根钉系统内固定。留置引流管引流。患者清醒后即感左下肢疼痛消失。术后第5天,伤口引流量24h内<30ml,拔除引流管,开始下地活动。术后10d行X线及CT检查,显示减压理想。术后3个月门诊复查,腰腿痛无反弹。摄片复查同前。继续随访中。
Castellvietal(1984年)根据腰椎X线片将腰骶移行椎分成4型,其中Ⅱ型为LSVT单侧(Ⅱa)或双侧(Ⅱb)横突同下方骶骨翼假关节。腰骶移行椎与骶骨间的间盘称移行间盘。移行间盘及紧邻上方椎间盘同时突出,未见明确报道。本例经CT及MRI检查明确CastellviⅡa型腰椎骶化并存L4~5及L5~S1椎间盘突出,经选择性神经根封闭明确均为责任节段,手术减压效果满意。
原始出处:
侯黎升, 白雪东, 葛丰, 等. Castellvi Ⅱa型腰椎骶化并L_(4~5)及L_5~S_1椎间盘突出1例. 《临床骨科杂志》2018年第04期
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#腰椎骶化#
83
#椎间盘突出#
68
#AST#
68
#腰椎#
68
#Cas#
59
学习了,谢谢分享
92